Blood:在CLL细胞中,FBXW7突变导致NOTCH1降解障碍而异常积累
2018-12-07 MedSci MedSci原创
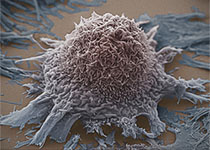
大约10%的慢性淋巴细胞白血病(CLL)患者携带NOTCH1突变,NOTCH1突变与预后不良相关。但是,NOTCH1激活可见于大概一半的CLL病例,即使没有NOTCH1突变,因此,可能存在其他因素干扰NOTCH1降解。E3泛素化激酶FBXW7负性调控NOTCH1,在2-6%的CLL患者中发生突变。目前这些突变导致的功能性后果尚不明确。Viola Close等人在36/905(4%)位未进行过治疗的
E3泛素化激酶FBXW7负性调控NOTCH1,在2-6%的CLL患者中发生突变。目前这些突变导致的功能性后果尚不明确。Viola Close等人在36/905(4%)位未进行过治疗的CLL患者中发现FBXW7突变,所有突变均为杂合突变。大部分是错义突变(78%),主要影响WD40底物结合结构域;10%的突变位于α-转录本的第一个外显子上。
为鉴别FBXW7在CLL中的靶蛋白,研究人员通过CRISPR/Case9建立WD40结构域截短体的CLL细胞系(HG-3)。纯合截短FBXW7会导致激活型NOTCH1-NICD和c-MYC蛋白水平增加,同时HIF1-α的活性也增强。芯片模型预测FBXW7-WD40结构域上的新突变G423V和W425C突变可改变蛋白底物的结合,而A503V突变没有影响。
通过对过表达FBXW7和NOTCH1进行免疫共沉淀验证了预测的结合差异。在来源于携带FBXW7突变的CLL患者的原代细胞中,激活型NOTCH1-NICD的水平升高,而且抑制翻译时蛋白水平仍保持稳定。此外,FBXW7突变与NOTCH1靶基因的表达增强同时发生。因此,CLL细胞的FBXW7突变可解释为何部分患者的NOTCH1信号失调。
Viola Close,et al. FBXW7 mutations reduce binding of NOTCH1, leading to cleaved NOTCH1 accumulation and target gene activation in CLL.Blood 2018 :blood-2018-09-874529; doi: https://doi.org/10.1182/blood-2018-09-874529
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Notch1#
33
#FBXW7#
41
#Notch#
39
#OTC#
30
好文,值得点赞,更值得收藏!慢慢领会学习的。给点个赞!
72