Cell Death Dis:幽门螺杆菌诱导的ADM表达促进胃炎发生发展
2020-04-03 MedSci原创 MedSci原创
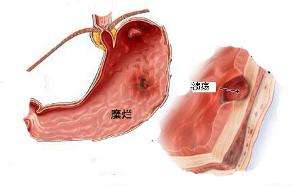
幽门螺杆菌(H.pylori)是一种革兰氏阴性细菌,全球半数以上的人均有感染。幽门螺杆菌是引起慢性胃炎、消化性溃疡及其他消化系统疾病的重要因素,并已被WHO列为I类致癌物。幽门螺杆菌感染后,胃上皮细胞
肾上腺髓质素(ADM)作为一种小的活性激素,是由52个氨基酸组成的多功能肽,在整个胃肠道中均有表达,但其与幽门螺杆菌诱导性胃炎的相关性目前仍不清楚。
在该研究中,研究人员发现幽门螺杆菌感染的患者及小鼠的胃粘膜的ADM表达水平升高。在幽门螺杆菌感染的人胃粘膜中,ADM的表达水平与胃炎的严重程度呈正相关;阻断ADM的表达可以减少幽门螺杆菌感染的小鼠胃黏膜内的炎症反应。在幽门螺杆菌感染期间,cagA依赖性的胃上皮细胞通过激活PI3K–AKT信号通路促进ADM的产生,导致胃粘膜内的炎症增强。该炎症的特征在于能够引起表达IFN-γ的T细胞增多,这些特征是由胃上皮细胞表达的ADM通过诱导AKT及STAT3的磷酸化而引起的。ADM还能够诱导巨噬细胞产生IL-12,并促进表达IFN-γ的T细胞的应答,从而促进幽门螺杆菌相关性胃炎的发生发展。因此,阻断或敲除IFN-γ能够减少幽门螺杆菌感染的小鼠胃粘膜内的炎症发生。
综上,该研究确定了一种新的调控网络,涉及幽门螺杆菌、胃上皮细胞、ADM、巨噬细胞、T细胞及IFN-γ,这些因素在胃部微环境中共同发挥了促炎症作用。
原始出处:
Kong et al. Helicobacter pylori-induced adrenomedullin modulates IFN-γ-producing T-cell responses and contributes to gastritis. Cell Death and Disease ( 2020) 11:189
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ADM#
53
#CEL#
55
#Dis#
53
#Cell#
58
#发生发展#
63
#螺杆菌#
40
#Death#
34