Lancet Respir Med:国际性多队列研究---中性粒细胞胞外陷阱与支气管扩张症的严重程度和治疗反应密切相关!
2021-02-23 MedSci原创 MedSci原创
NET是支气管扩张症病情严重程度和治疗反应的关键标志物
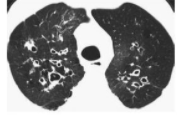
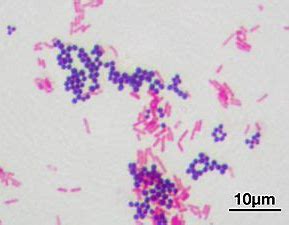
支气管扩张主要是一种中性粒细胞炎症性疾病。由于人们对导致严重疾病的潜在机制知之甚少,目前还没有直接靶向中性粒细胞炎症的既定疗法。中性粒细胞胞外陷阱(NET)形成是一种宿主防御方式,与多种炎症性疾病有关。
本研究目的是调查NET在支气管扩张症的严重程度和治疗反应中的作用。
在这项观察性研究中,研究人员首先使用液相色谱-串联质谱法在40位支气管扩张患者中筛查与疾病严重程度相关的蛋白质组生物标记物,然后在两组支气管扩张患者中验证了这些生物标记物(分别有175位和275位患者),最后调查了病原菌是否影响重度支气管扩张患者的NET量。
在另一项研究中,研究人员招募了20位支气管扩张急性加重的患者,予以静脉注射抗生素治疗14天,并用蛋白质组学方法鉴定与治疗反应相关的蛋白质。该队列的研究结果在同一家医院住院的独立患者队列(n=20)中得到了验证。
为了评估大环内酯类药物减少NET的潜在用途,研究人员还检查了两项大环内酯类药物长期治疗的研究,一项是针对支气管扩张患者(n=52),一项是关于哮喘患者(n=47)。
轻/重度支扩患者的蛋白质组学
痰液蛋白质组学证实,NET相关蛋白在支气管扩张患者中最丰富,也是与疾病严重程度最密切相关的蛋白。
NET浓度不同的患者的治疗预后
这一发现在两个观察性队列中都得到了验证,在这两个队列中,痰NET与支气管扩张严重程度指数、生活质量、未来住院风险和死亡率相关。在20名急性加重期的患者中,静脉注射抗生素治疗的临床反应与成功减少痰中的NET有关。
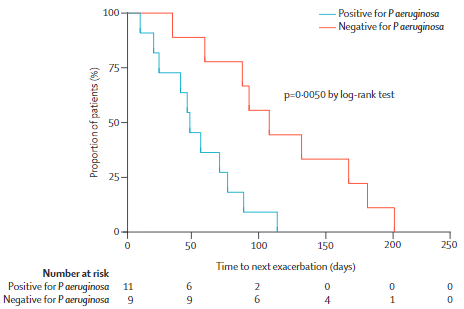
有无铜绿假单胞菌感染的患者预后
与非铜绿假单胞菌感染的患者相比,铜绿假单胞菌感染患者采用静脉注射抗生素治疗后的蛋白质组学变化和临床反应较轻,但对大环内酯类药物治疗有反应。小剂量阿奇霉素治疗与支气管扩张和哮喘患者在12个月内痰中NET显著减少有关。
因此,研究人员认为NET是支气管扩张症病情严重程度和治疗反应的关键标志物。本研究数据支持用现有的和新的疗法来靶向中性粒细胞炎症的概念。
原始出处:
Holly R Keir, et al. Neutrophil extracellular traps, disease severity, and antibiotic response in bronchiectasis: an international, observational, multicohort study. The Lancet Respiratory Medicine. February 17, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Lancet#
47
#支气管#
47
#扩张#
36
#中性粒细胞#
41
#中性粒细胞胞外陷阱#
54
#Med#
30
顶刊就是不一样,质量很高,内容精彩!学到很多
53