Eur Urol Focus:机器人辅助根治性前列腺切除术后尿失禁的预测
2021-04-29 AlexYang MedSci原创
已有研究表明,机器人手术期间记录的器械运动学指标可以预测尿失禁的结果。
已有研究表明,机器人手术期间记录的器械运动学指标可以预测尿失禁的结果。

最近,有研究人员评估了患者和治疗因素、外科医生效率指标和外科医生技术技能评分,特别是膀胱尿道吻合术(VUA),对预测机器人辅助前列腺根治术(RARP)后尿失禁恢复的模型的贡献。
研究人员收集了2016年7月至2017年12月进行的RARP的自动性能指标(APMs;仪器运动学和系统事件)和患者数据。研究结果发现,在115名接受RARP的患者中,89人(77.4%)的尿失禁康复,康复中位时间为166天(四分位数范围[IQR] 82-337)。23名外科医生进行了VUA手术。RACE评分的中位数是28/30(IQR 27-29)。在单个数据集中,技术能力(RACE)产生了最好的模型(C指数:CoxPH 0.695,DeepSurv:0.708)。在简略的APMs中,后部/前部VUA产生的模型性能优于其他RARP步骤(C指数0.543-0.592)。在详细的APMs中,针头驱动的指标产生了比其他缝合阶段表现更好的模型(C指数0.614-0.655)。另外,DeepSurv模型的表现一直优于CoxPH;两种方法在提供所有数据集时表现最好。局限性包括特征选择,这可能排除了相关信息,但预防了过度拟合。
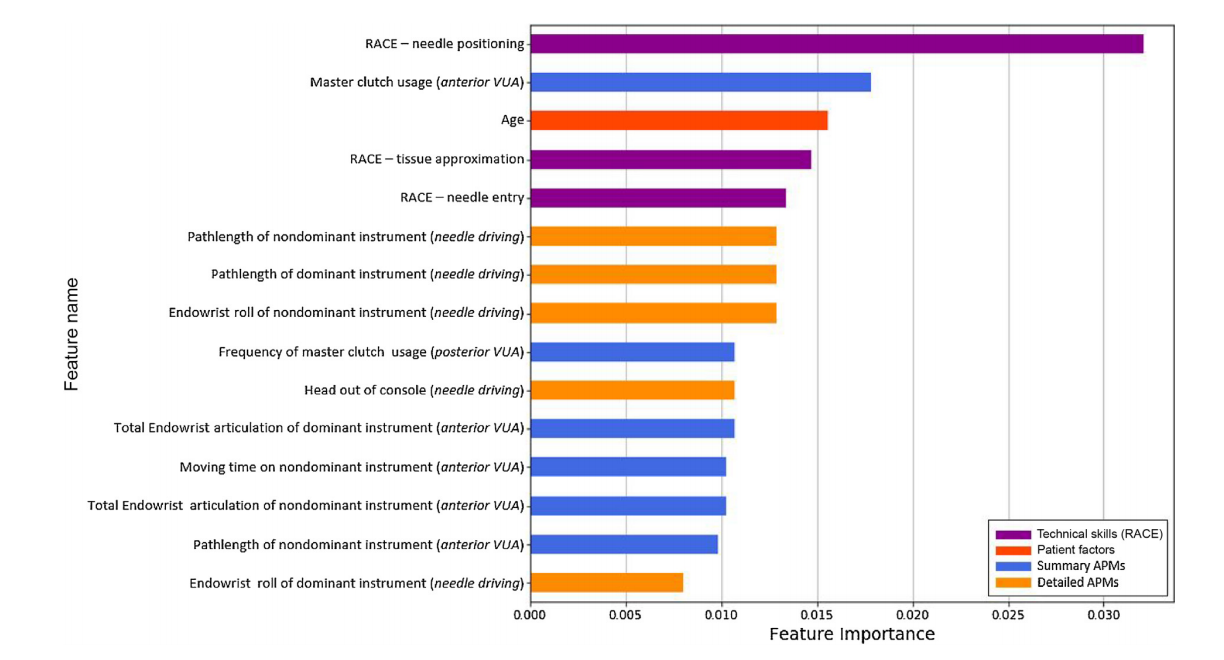
深度学习生存分析模型中特征重要性排序
最后,研究人员指出,VUA中的技术能力和 "针驱 "APMs是贡献最大的。表现最好的模型使用了所有数据集的协同数据。
原始出处:
Loc Trinh, Samuel Mingo , Erik B Vanstrum et al. Survival Analysis Using Surgeon Skill Metrics and Patient Factors to Predict Urinary Continence Recovery After Robot-assisted Radical Prostatectomy. Eur Urol Focus. Apr 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#前列腺切除#
38
#切除术#
29
#尿失禁#
45
#机器人#
38
#机器人辅助#
38
#机器#
34
#根治#
26