Chest:四种静脉维生素C给药方案在危重症患者的药代动力学分析
2018-03-07 xing.T MedSci原创
由此可见,2g/d的治疗剂量与正常血浆浓度相关,10g/d的治疗剂量与正常偏高的血浆浓度、增加的草酸盐排泄和代谢性碱中毒相关。持续治疗需要预防维生素缺乏症。
早期高剂量静脉注射维生素C正作为重症患者的辅助治疗进行研究,但最佳剂量和输注方法尚不清楚。近日,呼吸领域权威杂志chest上发表了一篇研究文章,该研究的主要目的是描述四种不同给药剂量方案的剂量-血浆浓度之间的关系和安全性。
该研究为四组随机药代动力学试验。患有多器官功能障碍的重症患者随机接受2g/天或10g/天的维生素C,以及每日两次静脉推注或连续输注48小时。终点是96小时内的血浆维生素C浓度,12小时尿排泄维生素C、草酸盐和碱过量。研究人员使用NONMEM开发人群药代动力学模型。
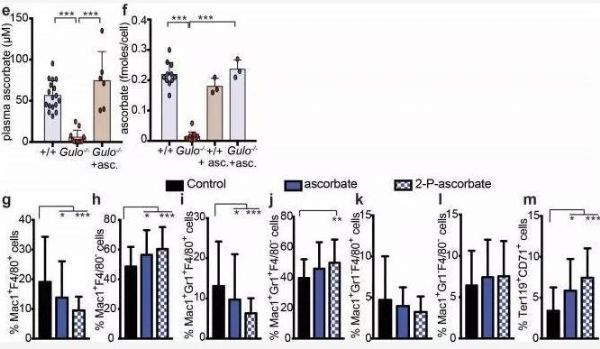
该研究纳入了20名患者。以肌酸酐清除率和体重作为独立协变量的二室药代动力学模型描述了四种方案中的最佳剂量方案。在2g/d的静脉推注下,1h时的血浆维生素C浓度为29-50mg/l,草酸盐浓度为5.6-16mg/l。在48h时,连续2g/d治疗组,稳态浓度为7-37mg/l。在10g/d的静脉推注下,1h的浓度为186-244mg/l,谷浓度为14-55mg/l。在48h时,连续10g/d,稳态浓度为40-295mg/l。 10g/d剂量组的草酸盐排泄和碱过量增加。停药后48小时,15%的患者血浆浓度降至维生素缺乏水平。
由此可见,2g/d的治疗剂量与正常血浆浓度相关,10g/d的治疗剂量与正常偏高的血浆浓度、增加的草酸盐排泄和代谢性碱中毒相关。持续治疗需要预防维生素缺乏症。
原始出处:
Harm-Jan de Grooth,et al. Vitamin-C pharmacokinetics in critically ill patients: a randomized trial of four intravenous regimens.chest.2018. https://doi.org/10.1016/j.chest.2018.02.025
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#EST#
33
#静脉#
35
#药代#
38
#给药方案#
33
#Chest#
34
#重症患者#
35
#药代动力学#
27
#危重症患者#
31
学习.谢谢分享.
62