Int J Cardiol:法洛四联症修复成人该如何选择运动训练?
2018-01-04 xing.T MedSci原创
由此可见,间歇训练和连续训练都是安全的。间歇训练似乎在改善运动能力、血管功能、NT-proBNP和纤维蛋白原水平方面更为有效,而连续训练似乎能更有效地改善心脏自主神经功能和QoL。
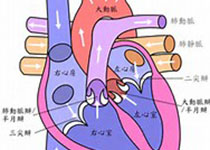
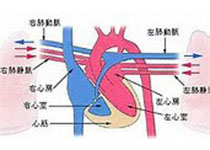
法洛四联症(ToF)修复的成年人运动能力、血管和心脏自主神经功能以及生活质量(QoL)受损。高强度间隔或适度连续运动训练对修复的ToF成年患者这些参数的具体影响仍然未知。近日,心血管领域权威杂志International Journal of Cardiology上针对这一问题发表了一篇研究文章。
30名成年ToF患者被随机分配到高强度间歇、中等强度连续训练(36组,每周2-3次)或常规护理(无监督训练)组。在基线和干预期后,研究人员测定了参与者运动能力、血流介导的血管舒张、脉搏波速度、NT-proBNP和纤维蛋白原水平、心率变异性和恢复以及QoL(SF-36问卷)。
27名患者(平均年龄为39±9岁,女性占63%,每组9名)完成了这项预研究。与没有运动的参与者相比,两个训练组至少对心血管健康的一些参数方面有所改善。间隔运动而不是连续训练可以改善VO2峰值(21.2至22.9ml/kg/min,P=0.004)、流量介导的血管舒张(8.4至12.9%,P=0.019)、脉搏波速度(5.4至4.8m/s,P=0.028)、NT-proBNP(202-190ng/L,P=0.032)和纤维蛋白原水平(2.67-2.46g/L,P=0.018)。相反,连续运动而不是间隔训练改善了心率变异性(低频0.32至0.22,P=0.039)、运动后2分钟心率恢复(40至47次搏动,P=0.023)和SF-36量表的心理部分(87至95,P=0.028)。
由此可见,间歇训练和连续训练都是安全的。间歇训练似乎在改善运动能力、血管功能、NT-proBNP和纤维蛋白原水平方面更为有效,而连续训练似乎能更有效地改善心脏自主神经功能和QoL。
原始出处:
Marko Novaković,et al. Exercise training in adults with repaired tetralogy of Fallot: A randomized controlled pilot study of continuous versus interval training.International Journal of Cardiology.2017. https://doi.org/10.1016/j.ijcard.2017.12.105
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Cardiol#
24
#运动训练#
32
#法洛四联症#
29
谢谢分享.
55
继续关注.
62
继续学习.
51