影像学在颈动脉粥样硬化斑块检查中的应用
2018-08-26 张冰 中华医学信息导报
脑血管病具有发病率高、致残率高、病死率高及复发率高的特点,严重影响国民健康和国家的健康战略。颈动脉粥样硬化易损斑块的破裂、栓塞、局部血栓形成以及造成的管腔狭窄、引起的血流动力学改变是引起缺血性脑卒中和短暂性脑缺血的重要危险因素。
动脉粥样硬化斑块在动脉粥样硬化的基础上形成,表现为动脉内-中膜的局限性非对称性增厚。病理过程分为3个阶段:脂纹形成、纤维斑块形成和粥样斑块。粥样斑块的管腔面为质硬的纤维结缔组织(包括大量的平滑肌细胞和细胞外基质),又称纤维帽;核心部分为质软的脂质、坏死崩解产物和钙盐成分;底部为新生的肉芽组织、少量的淋巴细胞和泡沫样细胞。斑块分为稳定性斑块和易损性斑块,其中易损性斑块具有薄纤维帽和大的脂质核心,容易发生斑块内出血、破裂、溃疡、局部血栓形成及斑块碎片栓塞远端血管,是造成缺血性卒中的罪魁祸首。但早期筛查、辨别及干预可明显降低发病风险。
随着影像技术的发展,目前已有多种检查手段可以满足临床需求,但也各有千秋。比较影像学则是解剖学、病理生理学及影像学的有机结合,通过分析疾病不同发展阶段同病异影、同影异病的特点,总结各种影像检查方法的利弊,从而为临床疾病诊断和治疗提供可靠、安全、经济、便捷的客观依据,帮医师和患者选择可以接受、对临床诊治指导价值最高的检查方法。现对颈动脉粥样硬化斑块中的常见检查方法介绍如下。
超声检查
超声检查(US)具有无创、无辐射、快捷便利且价格低廉、重复性好等特点,是各个级别的医院都可以开展的常规检查办法。US可以精确测量内-中膜厚度,早期评估颈动脉粥样硬化的程度。根据回声特点,斑块可以分为软斑块、硬斑块和混合斑块,其中软斑块为易损斑块。二维超声还能够对断面斑块大小、管腔狭窄程度进行初步测量。但由于斑块为不规则三维结构,常规超声无法对容积作精准的判断。随着超声技术和设备的进展,出现了一批新技术,如超声造影(CEUS)、血管内超声(IVUS)和三维超声(3DUS)等。
CEUS是静脉注射特殊的声学造影剂,待到达颈动脉斑块后通过谐波成像技术显示斑块内新生血管以评估斑块的易损性,可显着提高成像的敏感度和特异度。斑块内新生血管缺乏正常的血管结构,且脆性大、通透性高,容易出血并导致斑块破裂。斑块内新生血管密度越高,在超声造影上显示增强越明显。虽然CEUS具有较高的敏感性和特异性,但仍具有一定的局限性,如与操作者的水平显着相关、没有量化的评价标准、不能显示血管结构等。
IVUS在心内科冠状动脉中应用广泛,可对血管腔做360o横断面图像,可清晰显示血管壁及粥样斑块的形态。能精准测量管径及横断面积、判断血管狭窄程度和长度、且能早期发现血管重构现象、判断斑块成分、对血管狭窄支架成型术后支架贴壁情况也能提供非常好的信息。但IVUS空间分辨率较低,对太薄的纤维帽会做出误判。
3D-US 是通过图像采集及后处理来建立3D的解剖图像,可直观准确地显示斑块形态、位置、管腔狭窄程度、容积和斑块表面情况,还能动态观察治疗前后斑块容积的变化。但3D-US不能准确评估易损性斑块内部成分情况,对于极重度的狭窄(90%~99%)患者的二维图像采集欠佳,导致三维重建的结果受影响。
超声虽然具有诸多便捷的优点,但对颈内动脉颅内段显示较差,对于迂曲变异者的准确率较低,与CT血管造影(CTA)、磁共振血管成像(MRA)、数字减影血管造影(DSA)相比,其空间分辨率及组织分辨率不足。
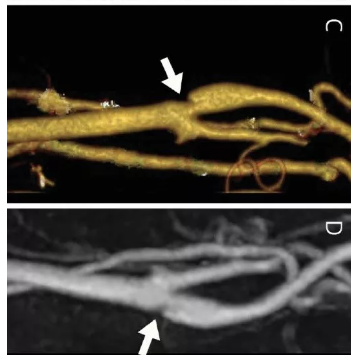
CT血管造影
随着CT设备的不断发展,目前CTA检查有更好的密度分辨率和空间分辨率,成像速度快、辐射损伤小、不受血流动力学影响,能清晰显示斑块的位置、大小、形态,还可以根据CT值分辨斑块的组成成分、评估斑块的易损性。CTA可准确区分软斑块和钙化斑,尤其对钙化斑较其他检查方法更敏感。但对于溃疡性斑块,CTA的检出率低于US和DSA。DeWeert等将CT值与病理结果对照研究后将CT值≤60 Hu界定为脂质斑块、60 Hu
磁共振血管成像
MRA可直观显示动脉管腔狭窄,还能显示管壁厚度及其与管腔的关系。对于重度狭窄及闭塞的管腔,三维动态增强MRA还能显示侧支循环建立情况。但MRA也存在以下缺陷:(1)费用较高;(2)成像时间长;(3)体内有金属异物会使检查受限;(4)因有容积放大效应,容易夸大狭窄程度;(5)难以鉴别严重狭窄和闭塞。
高分辨率MRI能对斑块成分作出精准判断,具有以下特点。
01纤维帽表现为斑块内层带样改变,T1加权像多为等信号,T2加权像和质子密度加权像多为信号强弱不定,而在飞行时间三维成像上多表现为低信号。因纤维帽富含新生血管,对比增强MRI不仅能评估斑块内新生血管,还能反映通透性参数,可更直观地显示其厚度及长度,也能更好地与不强化的脂质相鉴别。
02斑块内出血在各序列上主要表现为斑点、片状高信号。
03钙化在各序列上呈不规则低信号,斑块表面钙化由于流空效应在黑血序列上无法判断,在亮血序列上易于检测。
数字减影血管造影
D S A 一直被看作诊断血管病变的金标准。不仅能准确反映管腔狭窄和闭塞的范围及程度,还能清晰显示侧支循环情况。但DS A具有一定的创伤性、不能反映斑块内成分、对管壁厚度显示不佳;且在动脉粥样硬化早期可能由于血管重塑、斑块向管腔侧外移而造成对狭窄的低估。此外,DS A操作本身可以引起血管痉挛及卒中等并发症。
小结
张冰(湖州市中心医院神经内科)
对于颈动脉粥样硬化斑块的检查已有很多影像学手段,每种手段各有所长,也都存在一定的不足。目前,临床尚无单一的影像学方法能全面反映颈动脉粥样硬化斑块的真实情况,需要发挥比较影像学的优势,综合分析利弊,对多种方法进行协同利用,为临床疾病诊疗提供更合适、更可靠的依据。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#颈动脉#
26
#粥样硬化#
0
中文文章?
55
#斑块#
23
#颈动脉粥样硬化#
31
#动脉粥样硬化斑块#
31
学习了
47