Am J Psychiatry预防治疗物质使用障碍可降低饮食障碍患者死亡率
2021-11-09 自由影像之光 MedSci原创
SUDs对饮食障碍患者的额外死亡率有附加作用。因此,预防和治疗该患者组的SUDs对降低死亡率至关重要。
饮食失调与高死亡率相关。神经性厌食症(AN)是第二大致死性精神疾病,仅次于物质使用障碍(SUD)。神经性贪食症(BN)和饮食障碍患者的相应发病率较低,但仍显著升高,这突出了这些疾病的严重性。自2011年以来进行的研究证实了AN和BN的全因死亡率升高,而关于饮食障碍死亡率的研究(未另行说明)有限,无法复制先前的研究结果(5)。关于病因特异性死亡率,与普通人群相比,AN和BN患者的自杀率较高,其中AN患者的自杀率最高。其他研究表明,与普通人群相比,AN的外部(自杀、事故和凶杀)和内部(躯体和精神疾病)导致的死亡率都有所增加,其中外部原因导致的死亡率最高。关于不同类型的物质使用障碍(SUD)对整个饮食障碍的超额死亡率的贡献缺乏研究。
Angelina Isabella Mellentin等评估了酒精使用障碍和其他SUD与神经性厌食症、神经性贪食症和未指定饮食障碍的死亡率之间的关系,并与匹配的对照组受试者进行了比较。

该研究包括20,759名饮食失调患者和83,036名匹配的对照组受试者。计算危险比以比较饮食障碍患者和对照组(包括有和没有终身SUD诊断(滥用或依赖酒精、大麻或硬药物))之间的全因死亡风险。
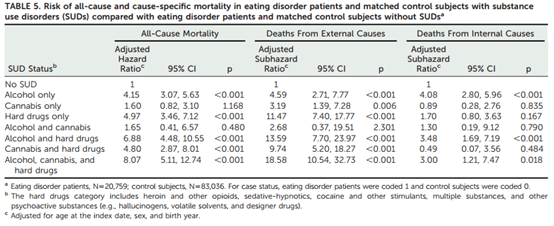
与滥用酒精和/或大麻(神经性厌食症、神经性贪食症和未指定饮食障碍患者的调整风险比分别为11.28 [95% CI=7.01, 18.16],5.86 [95% CI=3.37, 10.1]和10.86 [95% CI=6.74, 17.50]),或单独使用易成瘾毒品或与酒精和/或大麻联合使用的无SUDs的对照(95% CI = 2.43, 4.23), 1.24 (95% CI = 0.88, 1.77),和4.75 (95% CI = 3.57, 6.31))相比,每种类型的饮食障碍患者全因死亡的风险更高。与无SUDs的对照受试者相比,有SUDs的对照受试者也表现出全因死亡率升高的风险,尽管其程度远低于SUDs饮食障碍患者。
SUDs对饮食障碍患者的额外死亡率有附加作用。因此,预防和治疗该患者组的SUDs对降低死亡率至关重要。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#患者死亡#
31
#Psychiatry#
30
#物质使用障碍#
43
谢谢分享
49