J AM COLL RADIOL:如何让在缺血性卒中患者中争取影像学和急性治疗利用的社会公平?
2022-07-09 shaosai MedSci原创
健康差异指的是社会经济群体之间健康结果的可衡量的 "差异",而不公平一词表达的是 "不公正",特别是在医疗服务方面。
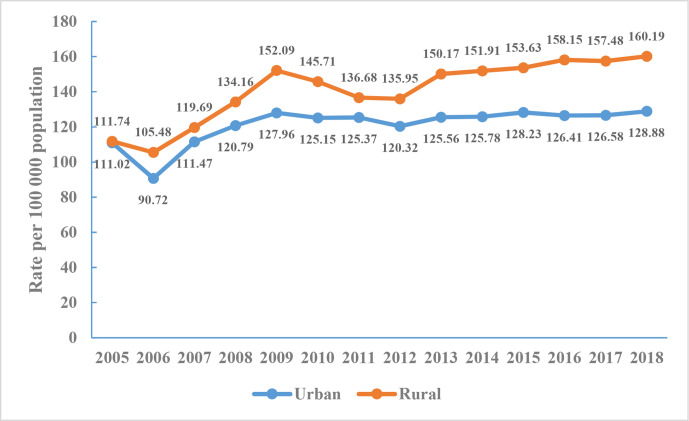
 据统计,在过去的十年中,卒中的总体死亡率有所下降,但仍然是死亡的主要原因之一,也是成年后致残的主要原因。然而,脑卒中患者在护理质量和临床结果方面仍存在社会经济水平上的显著差异。因此健康公平已成为卫生保健提供者和卫生保健系统的一个明确目标。
据统计,在过去的十年中,卒中的总体死亡率有所下降,但仍然是死亡的主要原因之一,也是成年后致残的主要原因。然而,脑卒中患者在护理质量和临床结果方面仍存在社会经济水平上的显著差异。因此健康公平已成为卫生保健提供者和卫生保健系统的一个明确目标。
造成健康差异和不平等的原因有很多。美国心脏协会发表了多份声明,强调了包括脑卒中在内的心血管疾病的种族差异和不平等,甚至呼吁对结构性种族主义采取行动,并将其作为健康差异的基本驱动力。健康差异指的是社会经济群体之间健康结果的可衡量的 "差异",而不公平一词表达的是 "不公正",特别是在医疗服务方面。
在评估医疗保健差异时,重要的是要考虑影响医疗保健资源的获取、供应和利用的患者、邻里和卫生系统层面的因素。尽管对卒中患者的影像检查和治疗是按照指南进行的,但护理的可变性和隐性偏见是存在的,有研究表明,不同人群对影像检查和治疗的利用不尽相同。在医院环境中,卒中患者在获得治疗方面存在社会经济差异。此外,社会经济地位低下的群体历来是最后受益于较新的医疗技术。
近日,发表在J AM COLL RADIOL杂志的一项研究探讨了从综合卒中中心(CSC)出院并被诊断为急性缺血性卒中患者在高级神经影像学和急性治疗利用方面是否存在社会经济差异,为减少患者的医疗差异、提高社会总体的医疗救治水平提供了参考。
本研究对某综合卒中中心2012年至2020年的连续急性缺血性卒中出院患者进行了回顾性研究。根据年龄、性别、种族、保险类型和社区级家庭收入中位数等社会经济因素,并评估了神经影像(CT血管成像[CTA]、CT灌注、MRI和MR血管成像[MRA])和急性治疗(静脉溶栓[IVT]和血管内血栓切除[EVT])利用率的差异。双变量分析采用了卡方检验。在控制卒中特定因素和合并症的情况下,进行多变量逻辑回归分析,以确定社会经济因素与神经影像学或治疗利用之间的关联。
在6140名缺血性卒中出院者中,在控制了卒中特异性因素和合并症后,种族和保险类型与神经影像学(CTA、CT灌注、MRI和MRA)或急性卒中治疗(IVT和EVT)的低利用率没有明显关系。然而,家庭收入中位数<80,000美元/年与较低的IVT使用有关(几率[OR],0.74;95%置信区间[CI],0.63-0.87)。此外,年龄≥80岁的人CTA(OR,0.62;95%CI,0.51-0.75)和EVT(OR,0.53;95%CI,0.39-0.73)使用率较低,女性的CTA(OR,0.78;95%CI,0.65-0.93)使用率较低。在亚裔(OR,1.33;95% CI,1.04-1.69)和无保险(OR,1.64;95% CI,1.07-2.50)的患者中,MRI的使用率明显较高;在私人保险的患者中,MRA(OR,1.24;95% CI,1.04-1.49)和EVT(OR,1.62;95% CI,1.20-2.20)明显较高。

图 在急性缺血性卒中研究人群中,使用逐步选择的逻辑回归与治疗利用相关的患者特征(2012-2020年,n=6140)
本研究表明,一旦克服就医障碍,急性卒中的影像和治疗方面的社会经济差异会大大减少。此外,放射科特有的因素可能会进一步减少卒中护理的差异,如提高成像效率和标准化的成像协议,因此值得进一步关注。
原文出处:
Jason J Wang,Artem Boltyenkov,Jeffrey M Katz,et al.Striving for Socioeconomic Equity in Ischemic Stroke Care: Imaging and Acute Treatment Utilization From a Comprehensive Stroke Center
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Coll#
37
#缺血性#
49
#缺血性卒中患者#
34
#卒中患者#
36
#缺血性卒#
46
好文章,谢谢分享。
34
#社会#
38