Radiology:哪种基底动脉闭塞机械取栓后预后好?
2019-08-14 shaosai MedSci原创
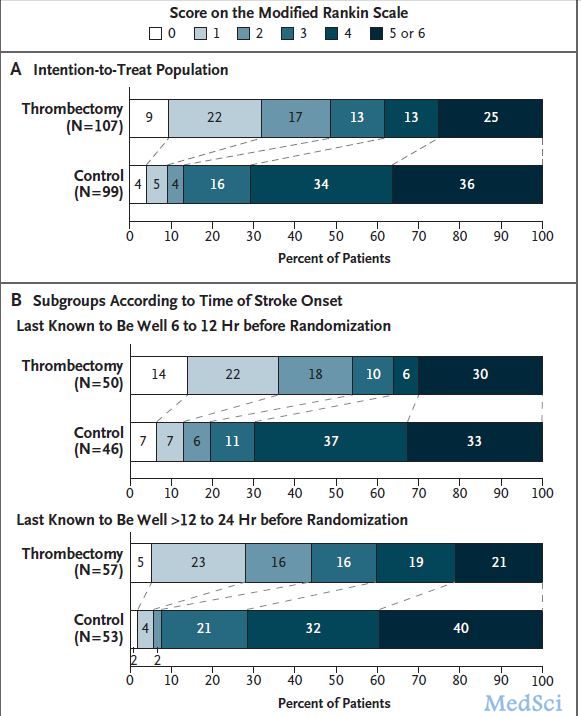
背景:由于基底动脉闭塞(BAO)所致急性脑卒中约占缺血性脑卒中的1%。然而,对于不同病理亚型的BAO脑卒中再通率和治疗结果尚不明确。本研究旨在比较不同BAO亚型经机械取栓后再通率和临床预后的差异。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#动脉闭塞#
33
#取栓#
41
#基底动脉#
42
#机械取栓#
59