Hypertension:减少钠盐摄入可降低交感神经血管转导活性
2019-03-06 国际循环编辑部 国际循环
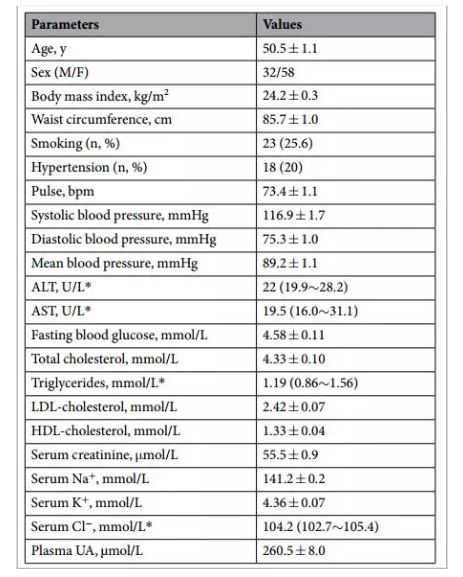
美国心脏协会(AHA)建议,成人全天理想钠盐摄入量不应超过1500 mg。但既往某些队列研究显示,低钠摄入可导致心血管死亡率增加,这可能与极低钠饮食(500 mg/d)引发肾素-血管紧张素-醛固酮系统的激活并刺激交感神经流出有关。目前,临床关于美国心脏协会推荐饮食对脉管系统交感神经调节作用的影响存在争议。近期,发表于Hypertension杂志的一篇研究对此展开讨论。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#TENS#
32
#盐摄入#
28
#钠盐#
33
#PE#
46
#Hypertension#
36