Gastric Cancer:术后并发症对胃癌患者生存结局的影响
2021-01-11 MedSci原创 MedSci原创
胃癌是第五种最常见的癌症,也是世界上与癌症有关的死亡的第三大主要原因, 外科手术切除是治疗晚期胃癌的最有效的手段,但是术后并发症会对患者的生活质量产生不利影响。
胃癌是第五种最常见的癌症,也是世界上与癌症有关的死亡的第三大主要原因, 外科手术切除是治疗晚期胃癌的最有效的手段,但是术后并发症会对患者的生活质量产生不利影响,甚至可能导致死亡,最近的研究发现术后并发症与胃癌术后患者的长期生存结果相关。虽然机理尚未完全阐明,但是很大的可能是残留的癌细胞的生长是通过手术应激或术后并发症造成的。本项研究旨在探究术后并发症对胃癌手术患者长期生存结局的影响,以及TMN分期为T3 / 4a局部晚期胃癌患者的囊肿切除术和非囊肿切除术对于生存期的影响。
该研究纳入1191名符合标准的患者。并发症通过Clavien-Dindo(CD)分类进行分级。通过使用Cox比例风险模型进行单变量和多变量分析,最后评估了并发症的等级(≥CD等级II或≥III等级)或类型(任何或腹腔内感染)对生存结果的影响。

研究人员发现胃癌手术后发生并发症(≥CD II级和≥III级)发生率分别为23.0%和9.7%,≥CDII级和CD≥III级腹腔内感染并发症的发生率分别为13.4%和6.9%。多变量分析显示,所有术后并发症都是整体生存的独立预后因素。相反,仅发现≥CD III级并发症是无复发生存的独立预后因素(危险比1.445;95%置信区间1.026-2.036;P = 0.035)。
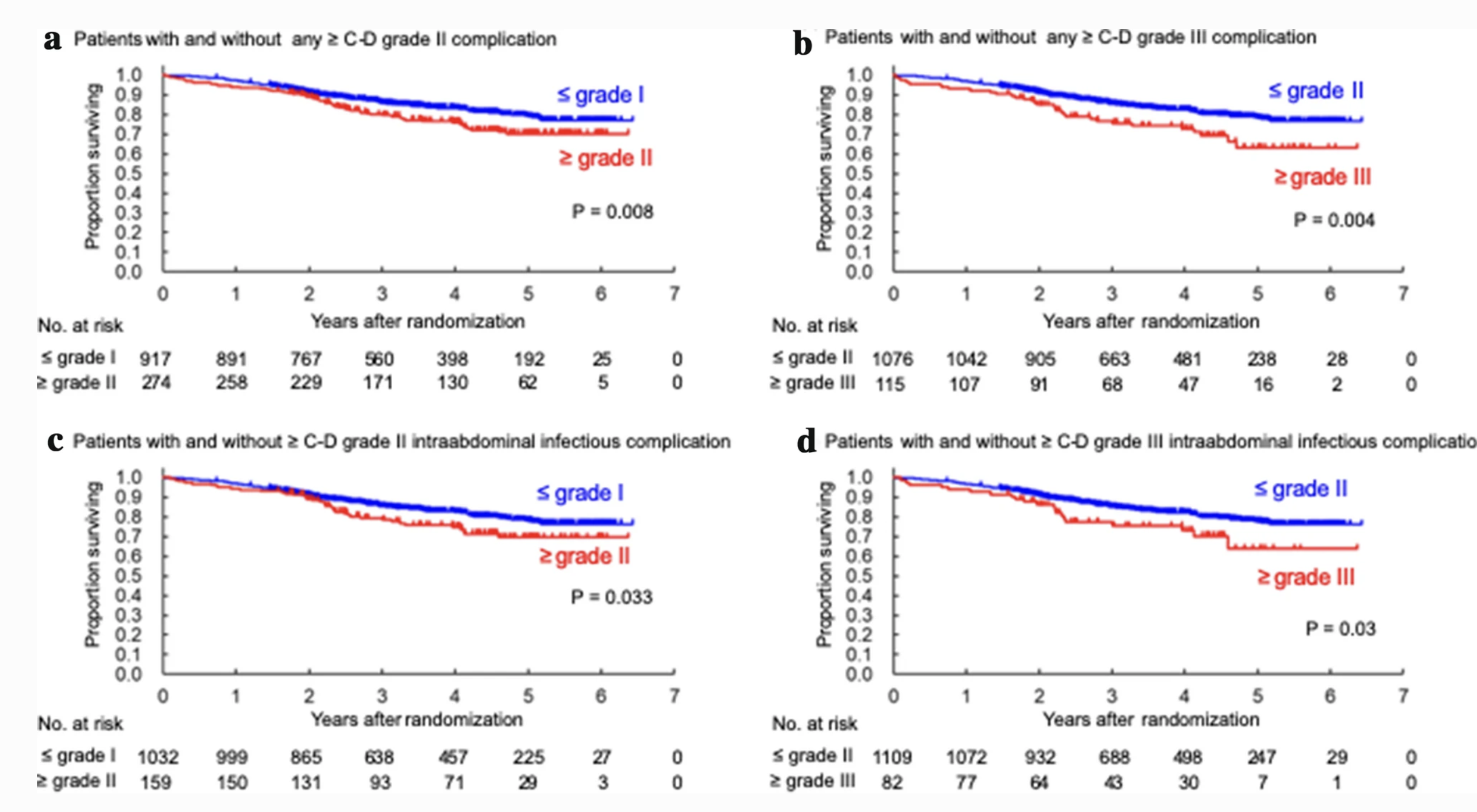
研究最后作者指出术后并发症会对cT3 / 4a胃癌患者的长期生存产生不利影响。任何≥CD III级并发症似乎都是预测阴性长期生存结果的最合适指标。
原始出处:
Masanori Tokunaga. Et al. Impact of postoperative complications on survival outcomes in patients with gastric cancer: exploratory analysis of a randomized controlled JCOG1001 trial. Gastric Cancer.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









外科手术切除是治疗晚期胃癌的最有效的手段
63
#胃癌患者#
55
学习
55
#并发#
49
#患者生存#
46
#GAS#
32
#gastric#
29
#AST#
16
胃癌#胃癌#
133
学习了
80