SCI REP:缺血性卒中或TIA患者收缩压与临床预后之间的相关性分析!
2017-10-25 xing.T MedSci原创
较高收缩压和较低收缩压与这一人群的预后不良有关。
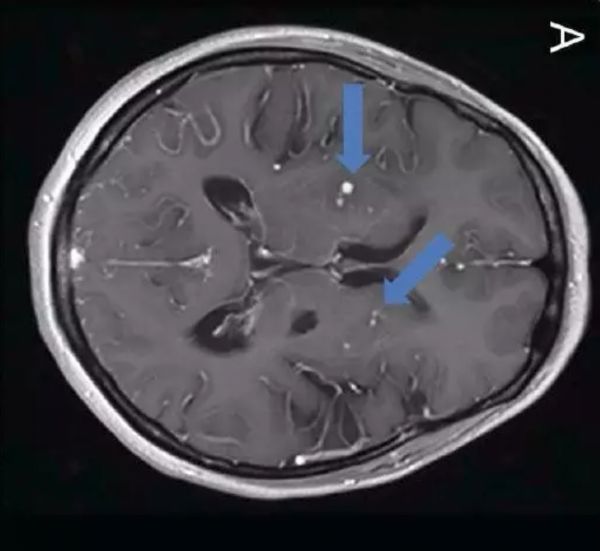
近日,Scientific reports 杂志上发表了一篇研究文章,研究人员的目的是通过参与缺血性卒中或短暂性脑缺血发作(TIA)患者血压和临床结局研究(BOSS研究)的2397名缺血性卒中或TIA患者收缩压(SBP)与临床结局之间的关系。
BOSS研究是一项以医院为基础的、前瞻性队列研究。受试者SBP定义为缺血性卒中或TIA发病后90天自我测量SBP的平均值。研究人员采用Cox比例风险模型对不同SBP分组的受试者联合的血管事件(CVE)和卒中复发风险进行了评估。研究人员采用限制性三次样条来探究收缩压与临床结局之间的关系。
研究人员观察到收缩压与CVE和90天内复发性卒中之间存在一个J型相关(非线性P<0.001)。在调整了年龄、性别、病史、心房颤动、入院NHISS评分和二级预防后,收缩压<115mmHg和⩾165mmHg与125-134 mmHg受试者者相比,对于CVE的风险比(95%可信区间)分别为3.45(1.11-10.66)和7.20(2.91-17.80),对于复发性卒中的风险比(95%可信区间)分别为2.68(0.75-9.53)和9.69(3.86-24.35)。在随访1年后,仍有类似的J形关系。
总之,较高收缩压和较低收缩压与这一人群的预后不良有关。
原始出处:
Xuewei Xie,et al. The J-curve Association between Systolic Blood Pressure and Clinical Outcomes in Ischemic Stroke or TIA: The BOSS Study.Scientific reports. 2017. https://www.nature.com/articles/s41598-017-10887-w
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#缺血性#
21
#收缩压#
37
#相关性#
29
#TIA患者#
37
#缺血性卒#
29
#相关性分析#
33
#临床预后#
20
较高收缩压和较低收缩压与这一人群的预后不良有关.
53
学习了.谢谢
40