ACR白皮书建议:警惕羟氯喹心脏毒性,心电图可帮助筛查!
2021-11-04 Shirley MedSci原创
10月26日,美国风湿病学会(ACR)发布白皮书,总结目前对羟氯喹(HCQ)/氯喹(CQ) 心脏毒性的认识,并基于共识提出了风险评估与监测指导。
羟氯喹(HCQ)和氯喹(CQ)是是治疗系统性红斑狼疮和类风湿性关节炎的药物。《2020中国系统性红斑狼疮诊疗指南》也建议SLE患者长期使用HCQ作为基础治疗。
10月26日,美国风湿病学会(ACR)发布白皮书,总结目前对羟氯喹(HCQ)/氯喹(CQ) 心脏毒性的认识,并基于共识提出了风险评估与监测指导。
由于在新冠疫情出有报告HCQ和CQ有潜在的抗冠状病毒活性,2020年初此药物的使用有所增加。虽然随机对照试验很快证实了这些治疗方法对COVID- 19无效。但是在此期间,已经多次报道患者的不良反应(包括心律失常和传导系统异常,以及心肌病)与HCQ/CQ使用有关。
HCQ/CQ的心脏毒
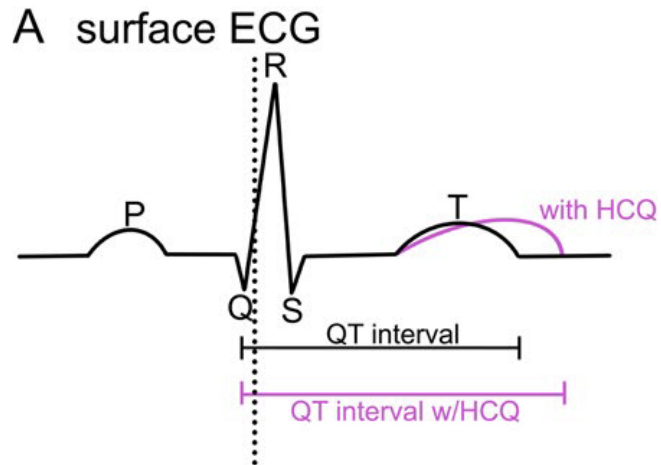
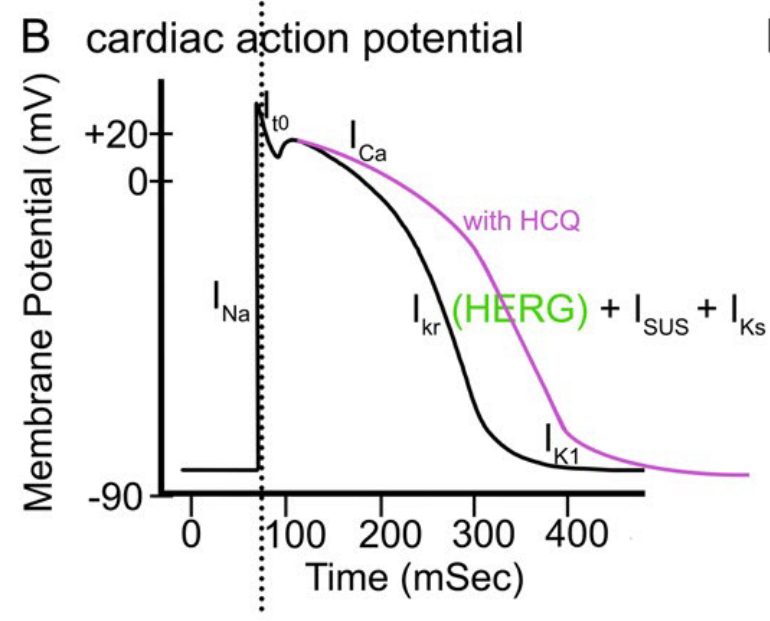
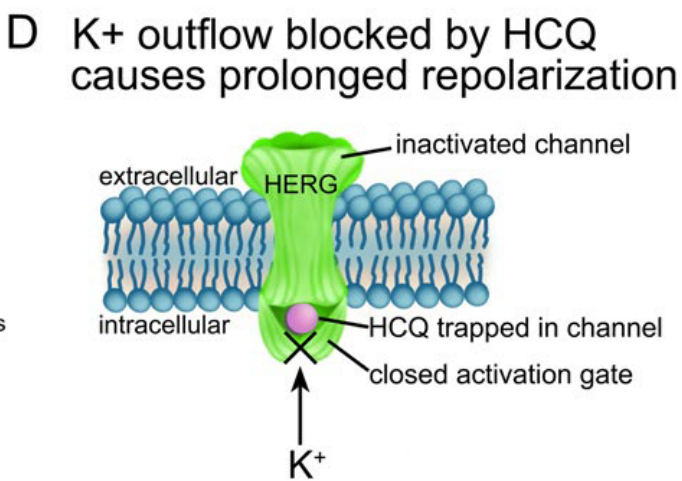
HCQ和CQ通过阻断钾外流通道与心室肌细胞相互作用,导致QT c延长。
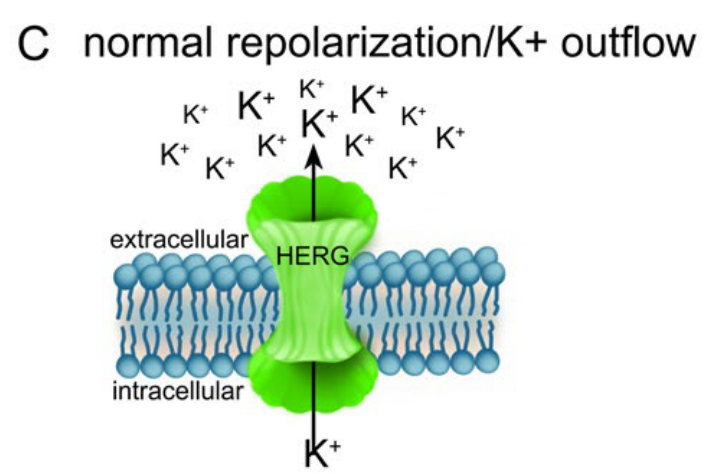
C:正常心肌细胞的复极是由钾离子通过HERG通道从细胞中流出。
D:HCQ或CQ会导致钾离子流出受阻
QT间期(简称QT)包括心室除极和复极激动时间,代表心室去极化和复极化过程的总时程,为自QRS波的起点至T波的终点所占的时间,测定值随年龄和性别而变化。QT间期延长会增加心源性猝死的风险,可能与QT间期延长与心尖扭转(一种罕见的多形性室性心动过速)有关。
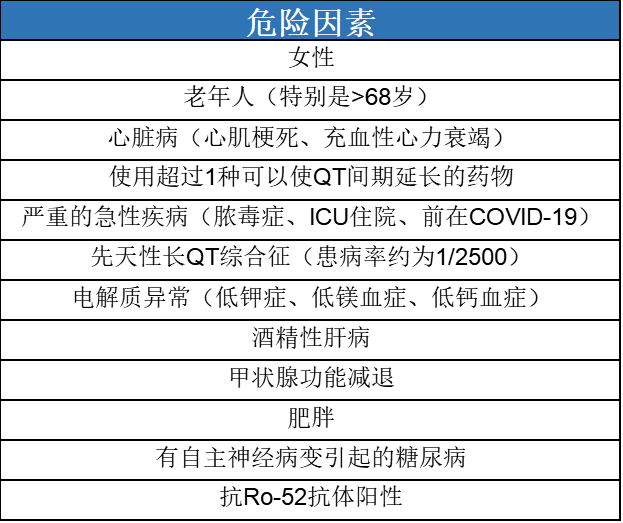
高风险人群
除了药物外,还有一些其他的因素会延长QT,医生应该注意这些高危因素,帮助患者及时规避风险,而有一些因素是可以被改变的,例如肥胖等。
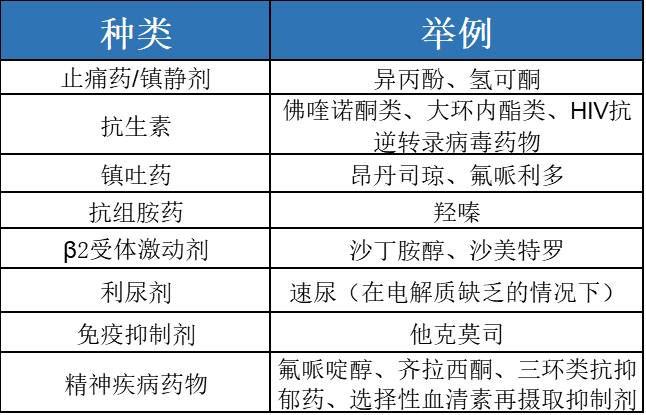
可以导致患者QTc延长的药物
如果患者有心律不齐的症状,如晕厥、晕厥前期或不明原因的头晕,应按照FDA标签建议进行包括心电图在内的心脏评估。对于接受过长期HCQ/CQ治疗并出现新的心脏症状的患者,医生应高度怀疑心肌病。如果发现没有其他病因的限制性心肌病,应考虑心肌内膜活检。

风湿病患者服用羟氯喹导致严重心律失常的发生率尚不清楚。大多数医生不会将心率失常和HCQ\CQ联系起来,所以应当有一部分患者被漏诊。建议对使用HCQ和QC的患者进行心电图筛查和随访,检测患者的心脏功能。
抗疟治疗在治疗SLE疾病中可以减少糖皮质激素的量、降低心血管疾病的风险、减少器官损伤和控制疾病。作为医生应当权衡药物对心脏的毒性,虽然药物收益远大于风险,但是也应该有关注药物毒性的意识。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#羟氯喹#
107
学到了
74
#ACR#
39
#白皮书#
48
xuxi
74