J Endod:数字根尖周X线影像和CBCT诊断天然和模拟牙根外吸收的准确性
2018-06-23 lishiting MedSci原创
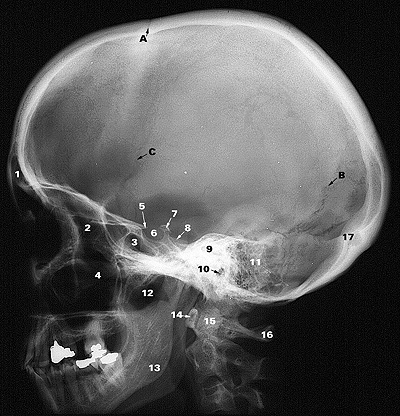
这篇研究的目的是为了比较数字化根尖周X线影像和锥形束CT(CBCT)对于诊断天然和模拟牙根外吸收(ERRs)的准确性及特异性,采用micro-CT影像分析作为对照标准。
这篇研究的目的是为了比较数字化根尖周X线影像和锥形束CT(CBCT)对于诊断天然和模拟牙根外吸收(ERRs)的准确性及特异性,采用micro-CT影像分析作为对照标准。研究使用SkyScan 1172 micro-CT scanner (Bruker microCT, Kontich, Belgium)对126颗牙齿进行扫描,采用NRecon software (Bruker microCT)对图像进行分析。Micro-CT影像分析后,将牙齿分为3组:对照组,42颗牙齿未有任何ERR;天然组,42颗牙齿存在1或多个ERRs;人工组,42颗没有ERR牙齿,人为制造孔洞以模拟ERR。随后,获取邻面、近中和远中的根尖X线片及CBCT影像,由2名专业的放射科医师进行双盲评估。结果显示,X线照相术和体层摄影术的敏感性和特异性分别为78.18%和97.27%以及59.52%和97.62%。个别组中,2种方法对天然和模拟的牙根吸收的检测敏感性和特异性均较低,并且存在统计学差异。结论:CBCT影像是检测ERRs最好的方式。数字根尖X线影像能够检测到的天然ERR缺隙仅有74.5%,而CBCT影像为94.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










好好学习天天向上
52
#准确性#
35
#X线#
35
#CBCT#
39
#牙根#
39
阅
54
很好
63