Nature:发烧改善自闭症?解释来了!
2019-12-22 Walter 转化医学网
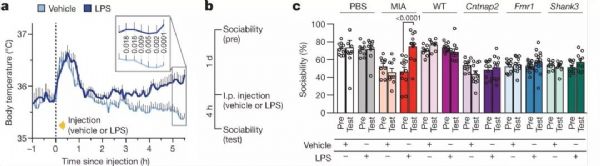
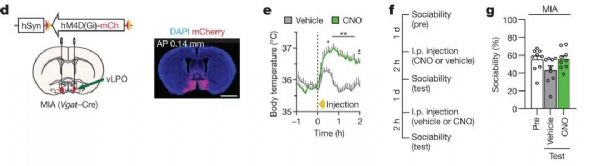
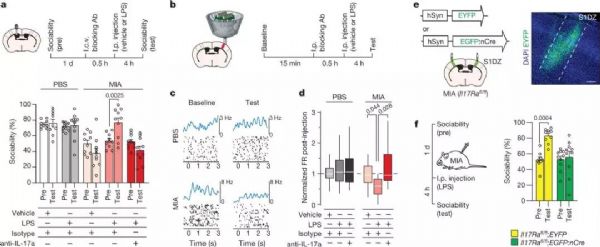
导 读:许多自闭症儿童的家长发现,孩子的社交障碍症状在发烧期间有所改善。这一奇特的现象吸引了众多研究关注。在过去15年中,至少有两组大范围调查证实这种情况的存在,但发烧和自闭症之间的具体联系仍尚未可知。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Nat#
36
#发烧#
50
#自闭#
35
好棒
106
学习了,学习了
110