Blood:Duvelisib相比奥法木单抗可显着提高RR CLL/SLL患者的无进展存活期和总体缓解率
2018-10-07 MedSci MedSci原创
中心点:与奥法木单抗相比,Duvelisib可显著提高RR CLL/SLL患者的无进展存活期和总体缓解率。摘要:Duvelisib(IPI-145)是一种口服的磷酸肌醇3-激酶(PI3K)δ和γ的双重抑制剂,现用于治疗恶性血液病。在克隆性B细胞恶性肿瘤中,如慢性淋巴细胞白血病(CLL)/小淋巴细胞白血病(SLL),PI3K-δ/γ信号可促进B细胞增殖和存活。在I期试验中,duvelisib在CLL
与奥法木单抗相比,Duvelisib可显著提高RR CLL/SLL患者的无进展存活期和总体缓解率。
摘要:
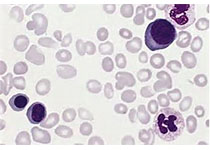
Duvelisib(IPI-145)是一种口服的磷酸肌醇3-激酶(PI3K)δ和γ的双重抑制剂,现用于治疗恶性血液病。在克隆性B细胞恶性肿瘤中,如慢性淋巴细胞白血病(CLL)/小淋巴细胞白血病(SLL),PI3K-δ/γ信号可促进B细胞增殖和存活。
在I期试验中,duvelisib在CLL/SLL患者中表现出临床治疗活性和可接受的安全性。研究人员随后在全球范围进行一随机III期试验,对比duvelisib和奥法木单抗单药治疗复发性/难治性(RR)CLL/SLL患者的疗效和安全性。
研究人员将受试患者按1:1随机分至duvelisib组(160人,25mg 2/日[BID])或奥法木单抗组(159人,静脉滴注[IV])。与奥法木单抗相比,duvelisib治疗可明显提高所有患者的无进展存活期(PFS:中位时间13.3个月 vs 9.9个月;HR 0.52,p<0.0001),包括具有高风险的染色体17p13.1缺失[del(17p)]和(或)TP53突变的患者(HR=0.40,p=0.0002)。采用duvelisib治疗的总体缓解率(ORR)也显著提高(74% vs 45%,p<0.0001),无论有无del(17p)。Duvelisib组最常见的副反应(AEs)为腹泻、中性粒细胞减少、发热、恶心、贫血和咳嗽;奥法木单抗组最常见的AEs是中性粒细胞减少和输液反应。
本试验结果表明duvelisib可作为RR CLL/SLL患者的潜在的有效的治疗选择。
Ian W. Flinn,et al. The phase 3 DUO trial: duvelisib versus ofatumumab in relapsed and refractory CLL/SLL. Blood 2018 :blood-2018-05-850461; doi: https://doi.org/10.1182/blood-2018-05-850461
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Duvelisib#
37
#存活期#
27
#CLL/SLL#
34