图文荟萃丨全面解读强直性脊柱炎
2022-04-18 风湿新前沿 梅斯医学
强直性脊柱炎(ankylosing spondylitis,AS)是一种主要侵犯脊柱,并可不同程度地累及骶髂关节和周围关节的慢性进行性炎性疾病。AS的特点为腰、颈、胸段脊柱关节和韧带以及骶髂关节的炎症
强直性脊柱炎(ankylosing spondylitis,AS)是一种主要侵犯脊柱,并可不同程度地累及骶髂关节和周围关节的慢性进行性炎性疾病。AS的特点为腰、颈、胸段脊柱关节和韧带以及骶髂关节的炎症和骨化,髋关节常常受累,其他周围关节也可出现炎症。
1、遗传:遗传因素在AS的发病中具有重要作用。遗传因素对AS易感性的影响最大。AS患者的一级、二级、三级亲属患病风险显著增加。目前已知与 AS 发生有关的基因有 100 多种。
2、感染:AS发病与感染密切相关,即诱导AS的发生(诱导)并影响疾病的进展及转归(驱动)。但是二者的因果关系尚未明确,究竟是感染触发了免疫反应还是携带HLA-B27遗传基因患者容易引起感染仍不十分清楚。
3、自身免疫:HLA-B27二聚体通过激活免疫机制的Th17通路启动全身免疫反应,使Th1/Th2比例失衡,进而导致AS发 生、发展。
4、其他:创伤、内分泌、代谢障碍和变态反应等亦被疑为发病因素。
中轴型脊柱关节炎的发病机制
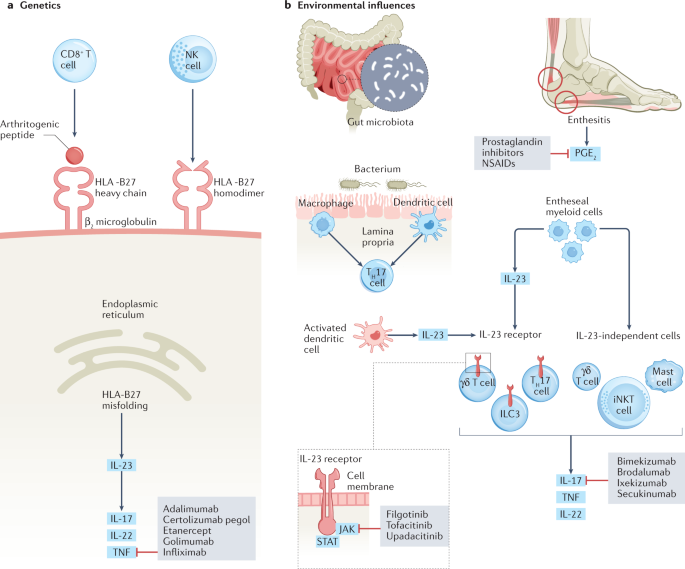
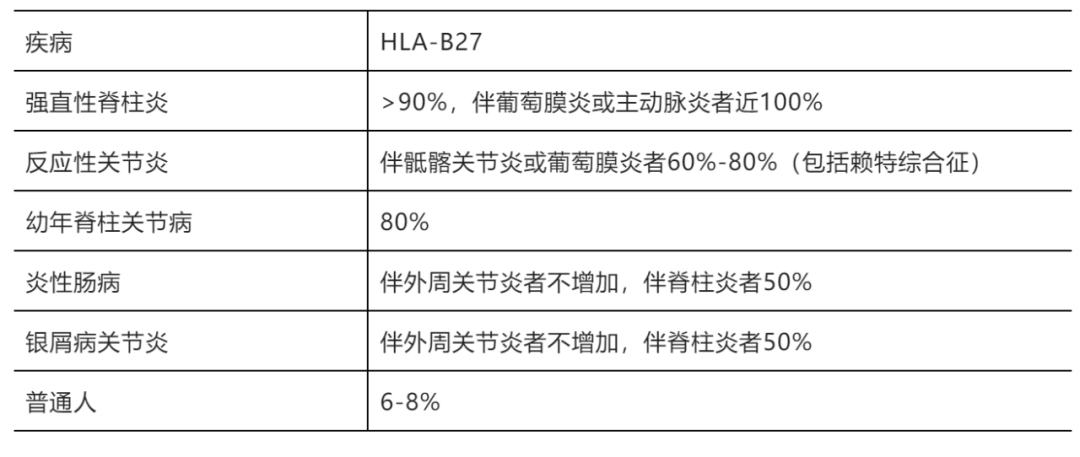
脊柱关节与HLA-B27
临床表现
1.关节表现
a) 早期腰骶、下腰背或者臀部酸痛,难以定位的钝痛。背部发僵,休息加重,轻微活动减轻,夜间疼痛明显,即“炎性疼痛”。
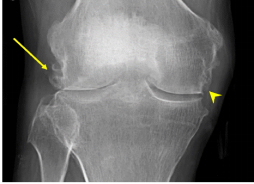
b) 外周关节首发症状为43%(积水潭实用骨科学),主要累及髋膝踝,非对称,发作与缓解交替。晚期髋关节屈曲挛缩,引起特征性固定步态,直立时膝关节被迫维持屈曲,以维持平衡。
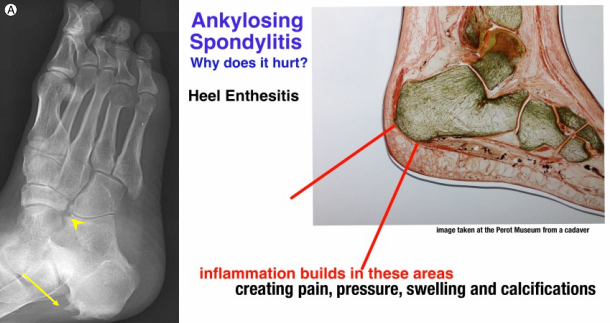
c) 关节外或者近关节处压痛,与肌腱止点病变相关。如:脊肋关节、脊柱棘突、肩胛、髂骨翼、股骨大转子,坐骨结节、胫骨隆突、足跟。
d) 累及中轴骨,并呈现向上发展趋势。对应部位疼痛,活动受限,胸廓扩张受限等。随着疾病进展,脊柱整个逐渐僵硬,出现腰椎曲度变平和胸椎过度后突。
2.关节外表现
a) 眼部疾病:急性虹膜睫状体炎或结膜炎(AS 伴葡萄膜炎的发生率高达 25%)
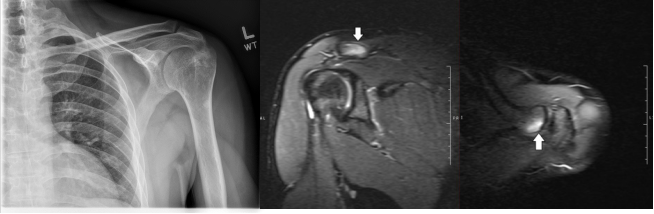
b) 心血管疾病:主动脉炎、主动脉瓣关闭不全、心脏传导系统受累
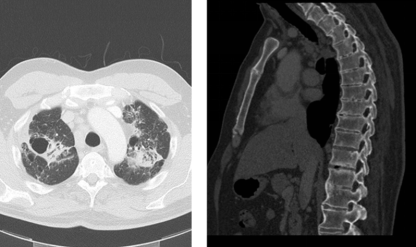
c) 呼吸系统:以顶叶/上叶为主的肺间质性疾病,可有囊肿形成与实质破坏
d) 肾继发损害:可表现为肾小球肾炎(IgA肾病)、肾淀粉样变性、非甾体类抗炎药相关性肾毒性(间质性肾炎、肾乳头坏死、急性肾损伤),生物制剂诱导的自身免疫性肾病等。
e) 马尾神经受侵犯:较罕见,目前为止尚无有效的治疗方法慢性附着炎可能引起硬膜囊薄弱,脊柱机械力传导致使硬脑膜扩张(见脊柱影像学改变)
诊断标准
1、1966年的AS纽约标准
有X片证实的双侧或单侧骶髂关节炎(按前述0-IV级分级),并分别附加以下临床表现的1条或2条,即:
①腰椎在前屈、侧屈和后伸的3个方向运动均受限;
②腰背痛史或现有症状;
③胸范围小于62.5px。
根据以上几点,诊断肯定的AS要求有:X线片证实的III~IV级双侧骶髂关节炎,并附加上述临床表现中的至少1条;或者X线证实的III~IV级单侧骶髂关节炎或II级双侧骶髂关节炎,并分别附加上述临床表现的1条或2条。
2、1984年修订的AS纽约标准
①下腰背痛的病程至少持续3个月,疼痛随活动改善,但休息不减轻;
②腰椎在前后和侧屈方向活动受限;
③胸廓扩展范围小于同年龄和性别的正常值;
④双侧骶髂关节炎II~IV级,或单侧骶髂关节炎III~IV级。如果患者具备④并分别附加①~③条中的任何1条可确诊为AS。
从上述2种标准可见,它们均缺乏对早期患者诊断的敏感性。为此,对一些暂时不符合AS诊断标准的患者,如其表现符合ESSG制订的脊柱关节病初步诊断标准,也可列入此类进行诊断和治疗,以免延误病情。
3、ESSG诊断标准
炎性脊柱痛或非对称性以下肢关节为主的滑膜炎,并附加以下任何1项,即:
①阳性家族史;
②银屑病;
③炎性肠病;
④关节炎前1个月内的尿道炎、宫颈炎或急性腹泻;
⑤双侧臀部交替疼痛;
⑥肌腱端病;
⑦骶髂关节炎。
符合者町列入此类进行诊断和治疗,并随访观察。
4、2009年ASAS推荐的中轴型SpA的分类标准
起病年龄<45岁和腰背痛≥3个月的患者,加上符合下述中1种标准:
①影像学提示骶髂关节炎加上≥1个下述的SpA特征;
②HLA-B27阳性加上≥2个下述的其他SpA特征。
其中影像学提示骶髂关节炎指的是:①MRI提示骶髂关节活动性(急性)炎症,高度提示与SpA相关的骶髂关节炎,或②明确的骶髂关节炎影像学改变(根据1984年修订的纽约标准)。
SpA特征包括:
①炎性背痛;
②关节炎;
③起止点炎(跟腱);眼葡萄膜炎;指(趾)炎;
④银屑病;克罗恩病,溃疡性结肠炎;
⑤对NSAIDs(NSAIDs)反应良好;
⑥SpA家族史;
⑦HLA-B27阳性;11CRP升高。
影像学诊断
骶髂关节影像学改变
-
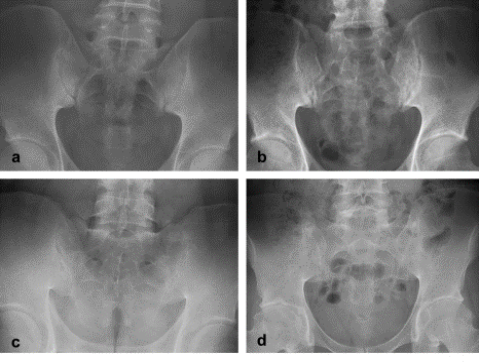
强制性脊柱炎导致骶髂关节炎通常——对称、双侧 -
早期骶髂关节间隙略增宽(初期关节面边缘变化轻微) -
进展阶段,关节边缘侵蚀样变化,可见硬化改变, 骶髂关节骶骨侧增生 -
最后骶髂关节完全融合 -
(见骶髂关节CT轴位像,X像) 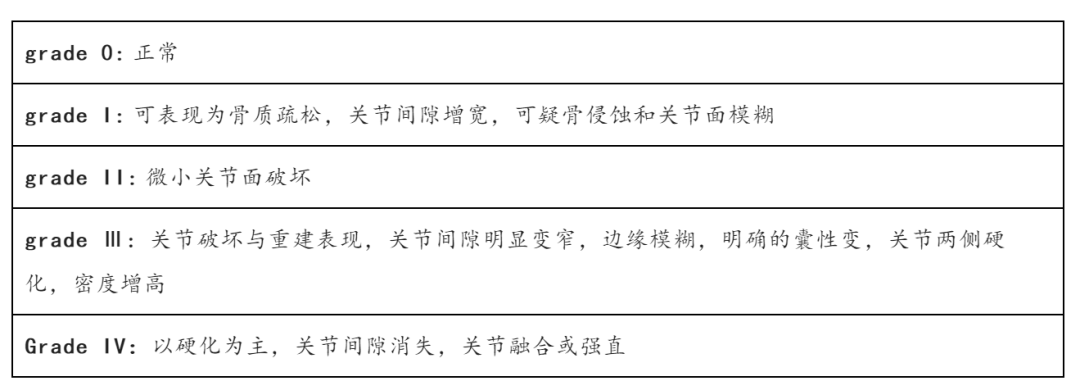
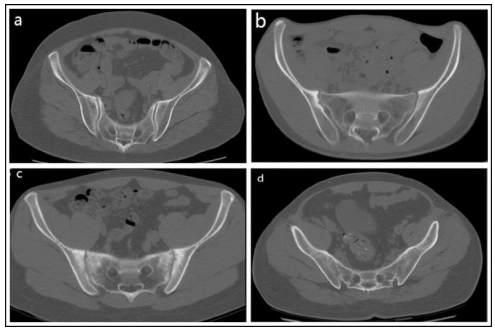
CT轴位图像上(骨窗)。(a)1级显示可疑改变(b)2级显示局部小面积糜烂或硬化,(c)3级显示明显异常糜烂、硬化,关节间隙缩窄(d)4级显示完全强直。
-
Romanus lesions代表炎性脊椎关节病的早期发现,如强直性脊柱炎和肠病性关节炎,并表现为累及椎体终板前后缘的不规则侵蚀。对这些炎症性侵蚀的愈合反应在影像学上表现为反应性硬化,这被称为shiny corner sign(图一)

(图一)AS患者(shiny corner sign,见) 对比正常脊柱侧位片(右侧)
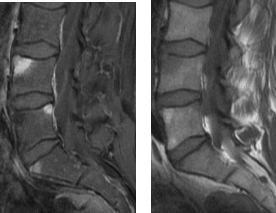
(图二)Sagittal T1 C+ fat sat(左)Sagittal T1(右):活动性炎症性改变,L4和S1前方(L5后方),侵蚀呈低密度改变称Romanus lesion
图三

图四

图五

图六
图七

图八

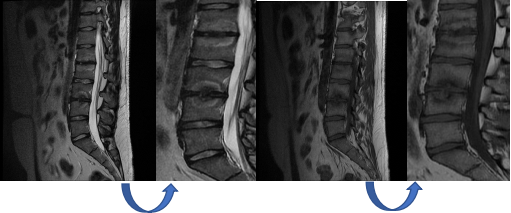
图九,强直性脊柱炎D11/12交界处假关节1例
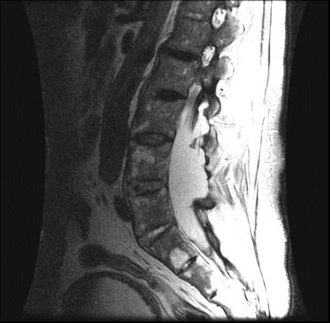
图十,腰骶椎矢状位T2加权MRI显示硬膜扩张。
图十一
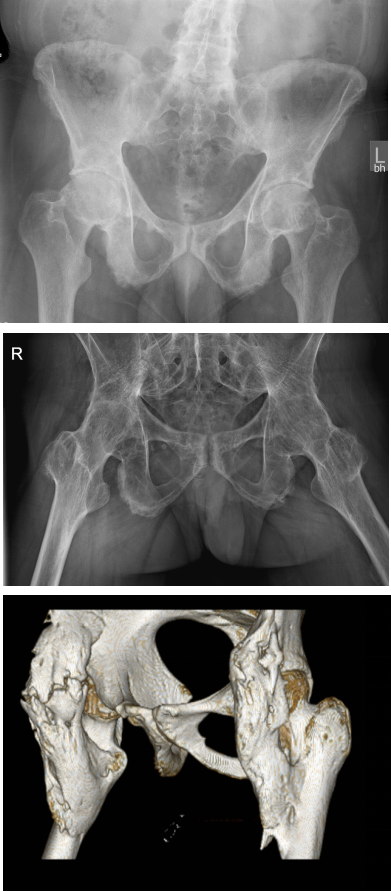
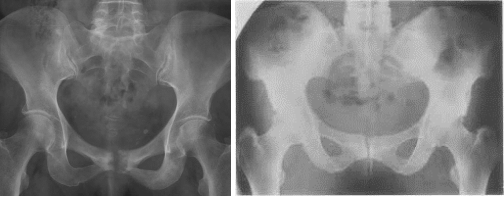
图十二。显示髋关节同心收窄、股骨头赘生物和软骨下硬化。髋关节不对称受累,右侧更明显。韧带止点骨化,特别是在坐骨结节处,呈现毛糙表现。骶髂关节近完全融合,伴耻骨联合糜烂性改变。中图,双侧髋关节骨性强直。下图,双侧髂肌部分骨中间肌异位骨化。
图十三
图十四
-
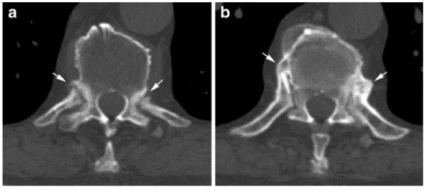
对骶髂关节X光片检查结果正常或不明确的患者可能有用 -
慢性炎症导致结构改变,如关节糜烂、软骨下硬化和骨强直,在CT上比在MRI或X线照片上更容易看到 -
一些正常的骶髂关节变异可能形似骶髂关节炎的特征 -
补充闪烁照相术以评估摄取增加的区域 -
在显示损伤方面优于X光片和MRI 晚期AS患者,怀疑颈椎骨折,CT成像模式选择较多,利于判断 由于轴位图像对横断面评估不佳,应获得矢状位重构图像
-
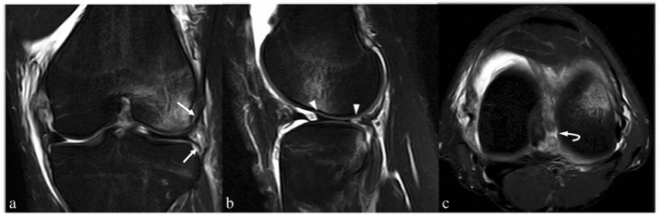
可在骶髂关节炎的早期诊断中起作用;MRI比CT或平片更敏感地检测炎症改变(在结构改变之前),如骨髓水肿(最好在STIR序列上显示)、滑膜炎和囊炎(在增强MRI T1加权序列上显示) -
MR显示滑膜强化提示与炎症活动性相关 -
棘间韧带增强提示有附着点炎 -
T2高信号提示:水肿或血管化纤维组织 -
在检测软骨炎症和破坏方面优于CT -
对活动性强直性脊柱炎患者疗效评估有帮助
-
可能有助于鉴别骶髂关节x光片表现正常或模棱两可的患者 -
由于在该位置的正常摄取放射性核素,定性评估可能很困难;因此,定量分析可能更有用 -
骶髂关节摄取1.3 : 1或更高的比值异常

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#荟萃#
69
#强直性#
58
比较全面
0
学习了
66
#脊柱炎#
48
学习了
72
认真学习~
76
学习!
87