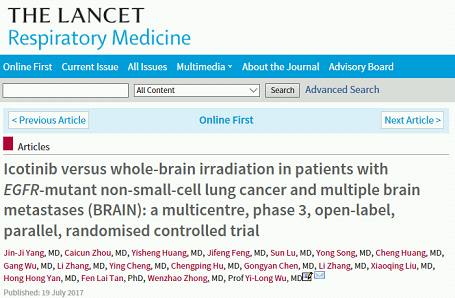
《柳叶刀》子刊发表研究成果,吴一龙教授点明NSCLC脑转移靶向治疗的未来探索方向
2017-07-24 佚名 肿瘤瞭望
7月19日,国际知名医学期刊《柳叶刀·呼吸医学》(The Lancet Respiratory Medicine)发表了由广东省人民医院吴一龙教授主持、国内众多专家联合开展的BRAIN研究结果。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#NSCLC脑转移#
31
#研究成果#
25
学习了分享了
74
学习了谢谢分享
76
学习下,向前辈学习
70
学习了,谢谢
82