Nat Med:转移性去势抵抗性前列腺癌治疗耐药性的相关研究
2021-03-11 xiaozeng MedSci原创
前列腺癌细胞状态取决于转录因子雄激素受体(AR)的活性,而后者是原发性和晚期疾病的主要治疗靶标。
前列腺癌细胞状态取决于转录因子雄激素受体(AR)的活性,而后者是原发性和晚期疾病的主要治疗靶标。目前对于转移性去势抵抗性前列腺癌(mCRPC)的治疗策略为第二代雄激素靶向疗法,包括恩杂鲁胺(enzalutamide)和阿比特龙(abiraterone)。
mCRPC通常是致命的,且会表现出对第二代雄激素靶向疗法的内在性或获得性抵抗力,对免疫检查点抑制剂的反应最小。然而,在癌症和免疫细胞中驱动耐药性的相关细胞程序仍知之甚少。
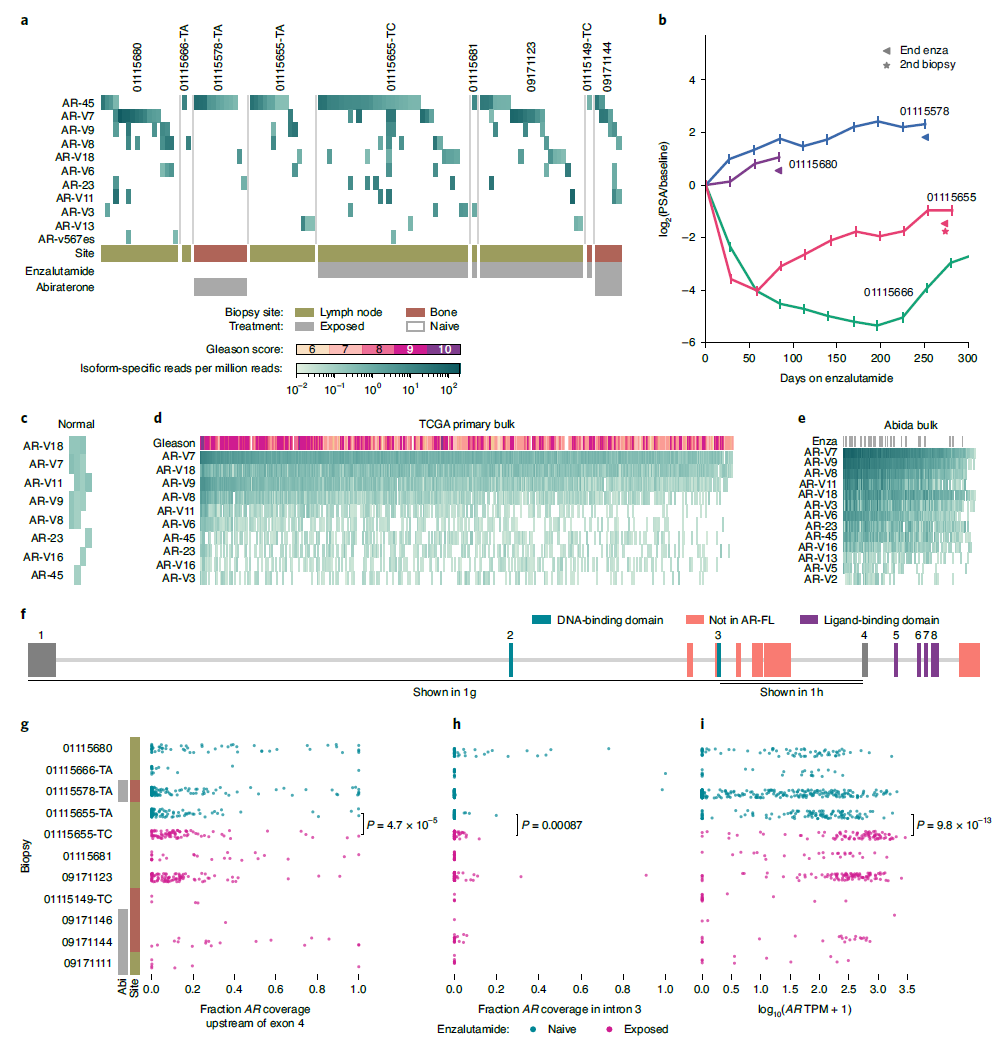
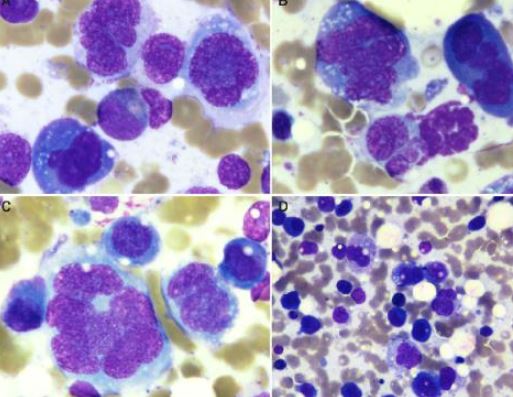
在该研究中,研究人员分析了来自14位晚期前列腺癌患者的涵盖所有常见转移部位样本(骨,淋巴结和肝脏)的单细胞转录组数据。结果显示,与治疗暴露无关,癌细胞普遍共表达多种雄激素受体亚型蛋白,包括被认为介导雄激素靶向疗法耐药性的截短体蛋白。
在不同疾病阶段和耐药状态中普遍共表达多种AR亚型
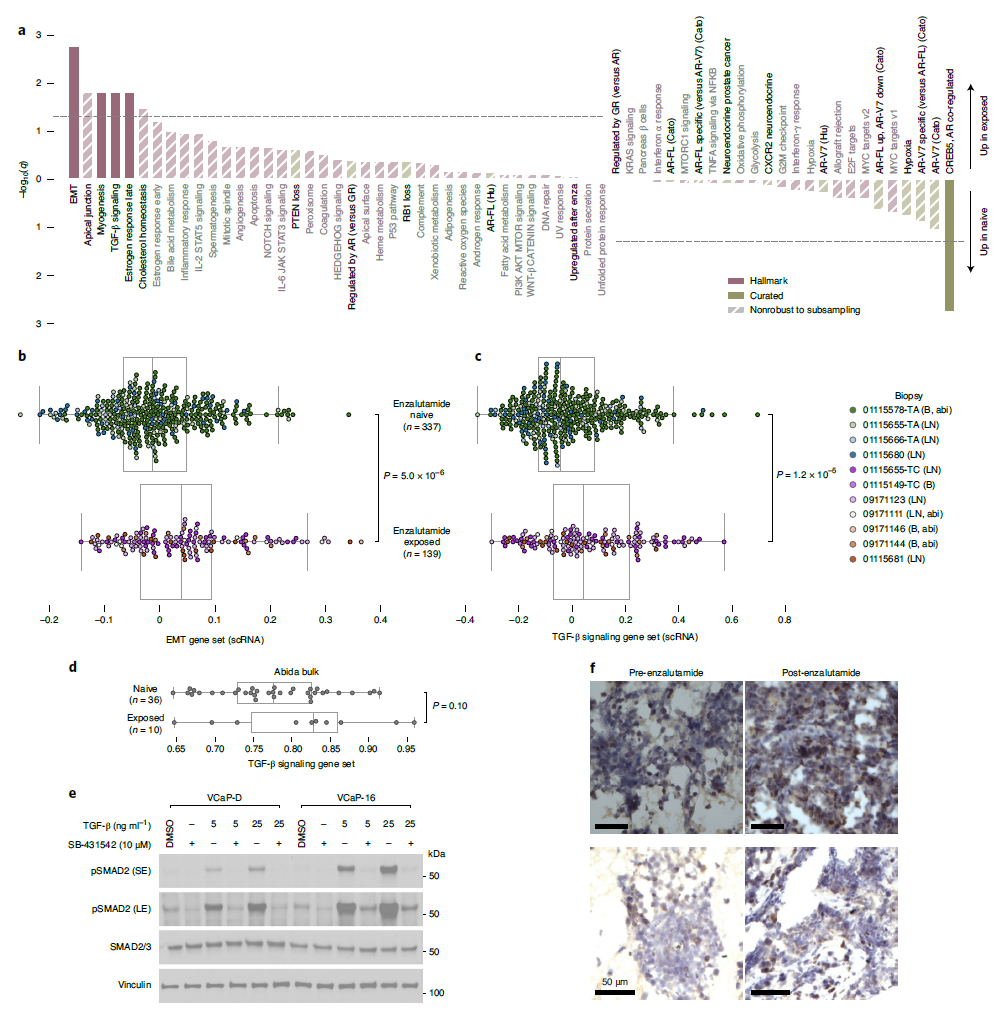
研究人员发现,恩杂鲁胺的耐药性与癌细胞固有的上皮-间质转化(EMT)进程和TGF-β信号转导通路相关。小细胞癌细胞显示出了不同的表达程序,这些程序由HOXB5、HOXB6和NR1D2以及转录调节因子促进可塑性所驱动。此外,一部分患者在恩杂鲁胺治疗后,克隆扩增的细胞毒性CD8+T细胞中的功能紊乱相关标志物呈现高表达。
恩杂鲁胺治疗的腺癌细胞中EMT和TGF-β相关信号上调
总而言之,该研究结果揭示了转移性去势抵抗性前列腺癌的癌症和免疫学特征,这些发现也为该疾病相关治疗策略的开发提供了一定的理论基础。
原始出处:
He, M.X., Cuoco, M.S., Crowdis, J. et al. Transcriptional mediators of treatment resistance in lethal prostate cancer. Nat Med (04 March 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#抗性#
46
#相关研究#
51
#Nat#
51
耐药性
74
#去势抵抗性前列腺癌#
0
#转移性#
29
#Med#
35
前列腺癌相关研究,学习了,谢谢梅斯
71
不错
88