Cell:科学家揭示端粒酶内部工作机制,在癌症、衰老中扮演重要角色
2018-06-23 佚名 细胞
为四膜虫结合端粒DNA的端粒酶的结构提供了机制上的新认知;关于其催化核心的完整结构揭示了一个叫做TRAP的新的结构单元;揭示了DNA从活性位点到端粒DNA结合p50-TEB复合物的详细途径;揭示了端粒酶RNA TRE模板-TBE在端粒DNA合成过程中的作用。
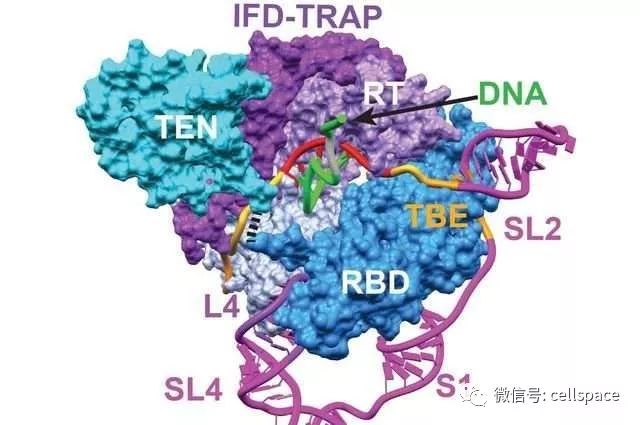
图片来源:Juli Feigon, et al./UCLA/Cell
端粒酶是一个RNA-蛋白复合物(RNP),负责使用其端粒酶逆转录酶(TERT)和包含模板的端粒酶RNA(TER)在染色体3’末端延长端粒DNA。它的活性是人类健康的关键决定因素,影响着衰老、癌症以及干细胞更新。但是由于缺乏端粒酶、尤其是结合着端粒DNA的端粒酶的原子模型,我们对端粒DNA反复合成的机制并不是很清楚。
为了解决这个问题,来自加州大学洛杉矶分校等单位的科学家们在Z. Hong Zhou及Juli Feigon的带领下使用冷冻电子显微镜揭示了四膜虫中结合了端粒DNA的活化端粒酶的原子结构,分辨率达4.8埃,相关研究成果于近日发表在《Cell》上,题为“Structure of Telomerase with Telomeric DNA”。
研究人员发现端粒酶的催化核心是一个由TERT和TER连锁的复杂结构,包括一个过去未完全表征的TERT结构域,可以与TEN结构域相互作用,在物理上封闭TER,以此调节其活性。
总的而言,这项研究揭示了端粒酶催化核心及其与端粒DNA相互作用形成的复合物的原子结构,为端粒酶组装和循环提供了新的观点,同时还为逆转录酶RNP提供了一个新的范例。这将为促进人们了解端粒及端粒酶在衰老、癌症等一系列生命过程中发挥的作用奠定基础。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#重要角色#
41
#CEL#
46
#Cell#
38
#工作机制#
36
#端粒酶#
43