Front Oncol:甲状腺激素比值对晚期转移性肾细胞癌患者的预后价值:来自Meet-URO 14研究
2021-11-26 yd2015 MedSci原创
研究表明,基线甲状腺激素受损(以低fT3/fT4比值为代表)是一线mRCC治疗患者的一个强有力的预后因素,且独立于目前临床实践中使用的其他参数。
甲状腺激素受损,表现为甲状腺激素水平的改变和较低的fT3/fT4比值,已经发现跟肿瘤和非肿瘤患者的较差预后相关。然而,基线甲状腺功能在转移性肾细胞癌(mRCC)患者中的作用尚未得到研究。近期,来自意大利的团队开展了相关研究,结果发表在Frontiers in Oncology杂志上。
研究收集意大利10个肿瘤单位的临床数据、基线生化结果和肿瘤预后。根据fT3/fT4比值值将患者分为三组,随后分析三组患者的无进展生存期(PFS)和总生存期(OS)的差异。还进行了单因素和多因素分析,以寻找PFS和OS的预后因素。
190名患者被纳入了ThreeFour研究,但只有134名患者有关于甲状腺激素的完整数据。因此,只有数据完整且有可能计算fT3/fT4比值的患者才符合分析条件。中位年龄为63.4岁,大约三分之一的患者年龄超过70岁。绝大多数患者为透明细胞癌而根据IMDC风险级别评为中度(61.2%)。一线治疗首选单药酪氨酸激酶抑制剂(TKI)( 78.4%),其次是免疫治疗和抗血管生成治疗联合(11.2%)和单独免疫治疗(10.4%)。
一线治疗期间,研究人员报告的最佳应答是62例病情稳定(46%),52例部分缓解(39%),16例疾病进展(12%);只有3例(2%)患者检测到完全缓解。在中位随访29.4个月后62例(46.3%)患者死亡。全人群中位PFS和中位OS分别为20.3个月(95% CI: 15-23.3个月)和49.4个月(95% CI: 40.9 66.8个月)。
基线fT3/fT4比值为0.13 ~ 4.87。在整个队列中,较高的fT3/fT4比值(被视为一个连续变量)与较好的PFS(HR=0.819,95% CI: 0.679-0.988)和OS(HR=0.672,95% CI: 0.492- 0.916)相关。
随后根据fT3/fT4比值将患者分为三组;0.266是低组和中间组的分界值,0.342是中组和高组的分界值。低、中、高fT3/fT4比值组的中位PFS分别为7.5、12.1和21.7个月(p<0.001)(中 vs 低fT3/fT4:HR=0.54,95% CI: 0.333-0.877; 高vs低fT3/fT4: HR=0.43, 95% CI: 0.263-0.693)。低、中、高fT3/fT4组的中位OS分别为6.5、48.6和70.5个月(p =0.006)( 中 vs 低fT3/fT4:HR=0.64,95% CI: 0.357-1.149; 高vs低fT3/fT4:HR=0.33, 95% CI: 0.171-0.625)。

PFS和OS
在单变量分析中,与PFS相关的特征包括从诊断到系统治疗的时间、fT3/fT4比值和IMDC风险分类。高中性粒细胞-淋巴细胞比值(NLR)、低fT3/fT4比值和中、低IMDC风险均与较差的OS相关。
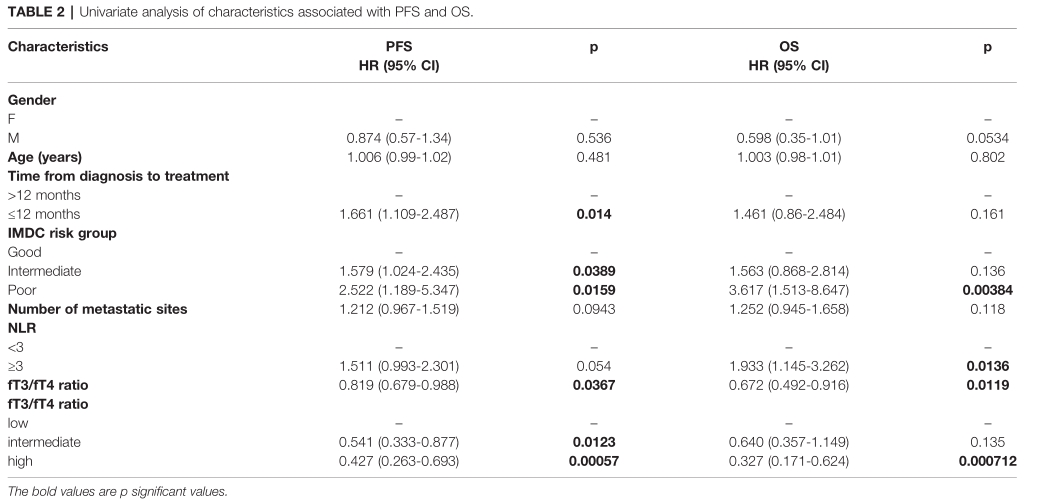
PFS和OS单因素分析
在多因素分析中,fT3/fT4比值是与PFS唯一仍有统计学差异的因素。高fT3/fT4比值和基于IMDC的低风险评分是与OS相关的因素。

PFS和OS多因素分析
低、中、高fT3/fT4比值组的DCR分别为77.8%,91.1%和95.5%(p=0.027)。治疗期间,患者在进行放射评估的同时进行甲状腺功能检查;其中69例发展为临床或亚临床甲状腺功能减退。与未发生甲状腺功能减退的患者相比,发生甲状腺功能减退的患者PFS和OS没有显著差异(中位PFS 11.9 vs 13.3个月,p=NS;中位OS 48.6 vs 54.9个月,p=NS)。
综上,研究表明,基线甲状腺激素受损(以低fT3/fT4比值为代表)是一线mRCC治疗患者的一个强有力的预后因素,且独立于目前临床实践中使用的其他参数。
原始出处:
Maruzzo M, Verzoni E, Vitale MG, Dionese M, Buti S, Galli L, Zivi A, Watutantrige-Fernando S, Zielli T, Zanardi E, Sabbatini R, Basso U, Zagonel V and Procopio G (2021) Prognostic Value of Thyroid Hormone Ratio in Patients With Advanced Metastatic Renal Cell Carcinoma: Results From the Threefour Study (Meet-URO 14). Front. Oncol. 11:787835. doi: 10.3389/fonc.2021.787835
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Oncol#
41
#细胞癌#
40
#晚期转移性肾细胞癌#
46
#预后价值#
49
#转移性#
31
#转移性肾细胞癌#
42
学习
51
学习了
61