Circulation Research:白细胞介素-6预测颈动脉斑块的严重程度、易损性和进展
2022-06-18 MedSci原创 MedSci原创
循环IL-6水平可预测颈动脉斑块的严重程度、易损性和进展。以2.0pg/mL临界值可以帮助识别可以从抗IL-6药物进行脑卒中预防治疗中受益的个体。
白细胞介素-6(IL-6)在动脉粥样硬化的病理生理过程中具有重要作用。
为了明确抗IL-6治疗是否可以作为颈动脉粥样硬化患者的卒中预防策略,近日,心血管领域权威杂志Circulation Research上发表了一篇研究文章,研究人员在以前瞻性人群为基础的心血管健康研究(CHS)中,评估循环IL-6水平是否可以预测颈动脉斑块的严重程度、易损程度和进展。

研究人员分别在基线和5年时对受试者进行了颈动脉超声检查。根据北美症状性颈动脉内膜切除术试验的狭窄程度评分,研究人员将受试者基线斑块严重程度评分为0-5分。斑块易损性是指存在明显不规则形状、溃疡或回声斑块。斑块进展5年后,狭窄程度增加≥1分。研究人员采用多变量线性(严重程度)或logistic(易损性和进展)回归建模来评估基线血浆IL-6水平与斑块特征之间的关系。此外,研究人员将动脉粥样硬化危险因素作为自变量。为了评估模型的稳定性,研究人员计算了未测量的混杂因子与log IL-6的关联的e值或最小强度(比值比量表)。
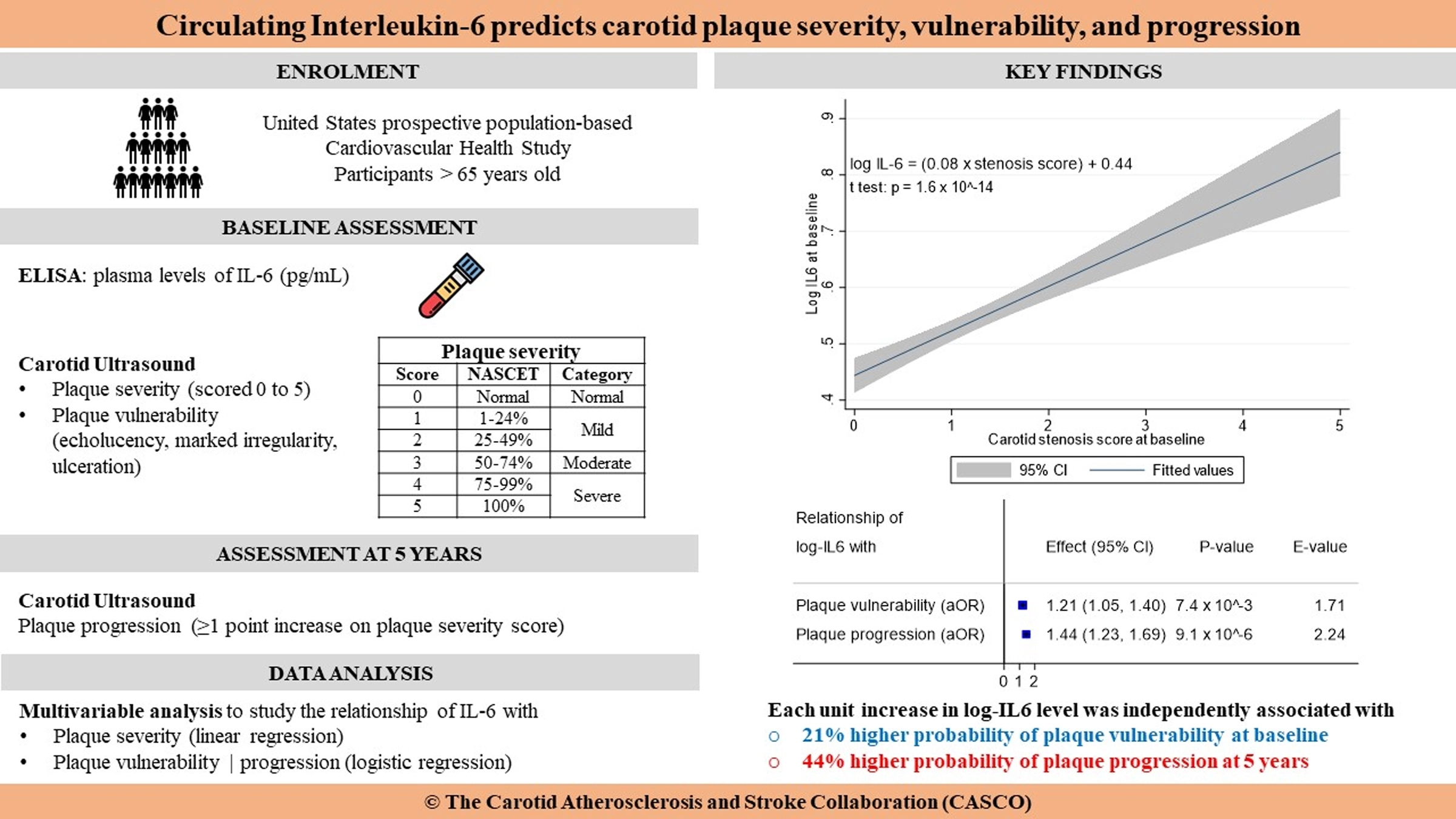
4334名受试者数据完整(58.9%为女性,平均年龄为72.7±5.1岁),其中1267名(29.2%)患者为易损斑块,1474名(34.0%)患者存在斑块进展。Log IL-6可预测斑块的严重程度(β=0.09,P=1.3×10−3)、易损性(OR为1.21[95%CI为1.05-1.40];P=7.4×10−3,E值=1.71)和进展(OR为1.44[95%CI为1.23-1.69],P=9.1×10−6,E值=2.24)。在斑块进展预测几率超过50%的参与者中,IL-6的平均log为0.54,对应浓度为2.0pg/mL。IL-6水平的二分法不影响预测模型的性能。
由此可见,循环IL-6水平可预测颈动脉斑块的严重程度、易损性和进展。以2.0pg/mL临界值可以帮助识别可以从抗IL-6药物进行脑卒中预防治疗中受益的个体。
原始出处:
Joseph Kamtchum-Tatuene,et al.Interleukin-6 Predicts Carotid Plaque Severity, Vulnerability, and Progression.Circulation Research.2022.https://www.ahajournals.org/doi/10.1161/CIRCRESAHA.122.320877
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













持续关注
47
#颈动脉#
58
#颈动脉斑块#
0
#斑块#
43
#Research#
49
#白细胞介素#
38