Clin Cancer Res:晚期肾细胞癌患者免疫治疗停药后的无治疗生存期(TFS):Check- Mate 214研究
2021-12-01 yd2015 MedSci原创
研究表明,晚期肾细胞癌患者(aRCC)一线nivolumab + ipilimumab治疗患者较舒尼替尼治疗获得更长的无治疗生存期(TFS)。
随机III期Check- Mate 214研究(ClinicalTrials.gov, NCT02231749)的结果显示,在有IMDC中度或不良预后风险的晚期肾细胞癌(aRCC)患者中,nivolumab联合ipilimumab治疗较舒尼替尼延长患者OS。近期,有研究提出无治疗生存期(TFS)来描述ICI治疗结束后直到开始后续全身治疗或死亡期间的抗肿瘤活性和毒性。Check- Mate 214研究42个月更新结果发表在CLINICAL CANCER RESEARCH杂志上。
TFS是通过随机分组中至42个月内(Kaplan Meier曲线之间的面积定义)来估计的:从随机化开始至方案治疗停止的时间和从随机化开始至开始后线治疗或死亡的时间。根据≥1例患者发生≥3级治疗相关不良事件(TRAE),TFS被细分为有毒性和无毒性TFS。
在847例IMDC中度或不良预后风险aRCC患者中,Kaplan Meier评估随机分组后42个月的OS nivolumab联合ipilimumab组为52%,舒尼替尼为39%。分别为31%和9%的患者未接受后续治疗,14%和4.1%的患者继续接受指定方案治疗。42个月TFS率分别为18%和4.9%。
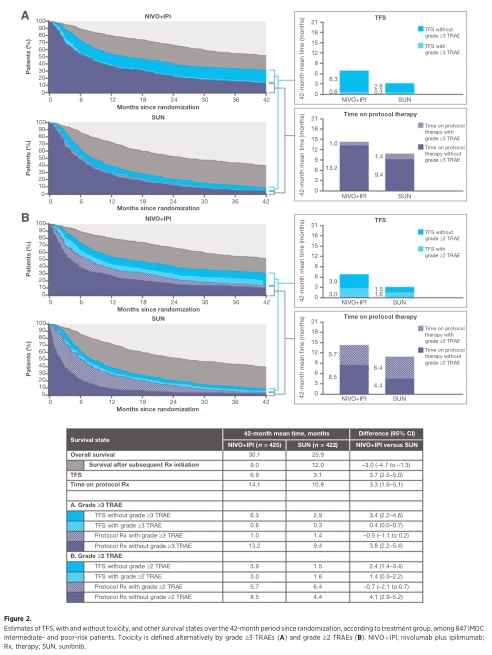
总体人群TFS对比
Nivolumab + ipilimumab的42个月中位TFS为6.9个月,而舒尼替尼为3.1个月[差异,3.7个月(95%CI,2.5 5.0)]。
基于毒性定义,nivolumab + ipilimumab的42个月平均TFS是舒尼替尼的两倍多[无≥3级TRAE的TFS:差异,3.4个月(95% CI, 2.2 4.6);无≥2级TRAEs的TFS:差异2.4个月(95% CI, 1.4 3.4)]。
在249名IMDC预后风险良好的患者中,70.1%的nivolumab + ipilimumab和73%的舒尼替尼患者存活,29%和24%的患者无需开始后续治疗,9.6%和15%的患者仍在方案治疗;因此,在随机分组后42个月,分别有19.5%和8.8%的患者无治疗生存。nivolumab加ipilimumab的42个月平均TFS大约是舒尼替尼的3倍长[11.0个月vs. 3.7个月;差异为7.3个月(95% CI, 4.6个月)]。
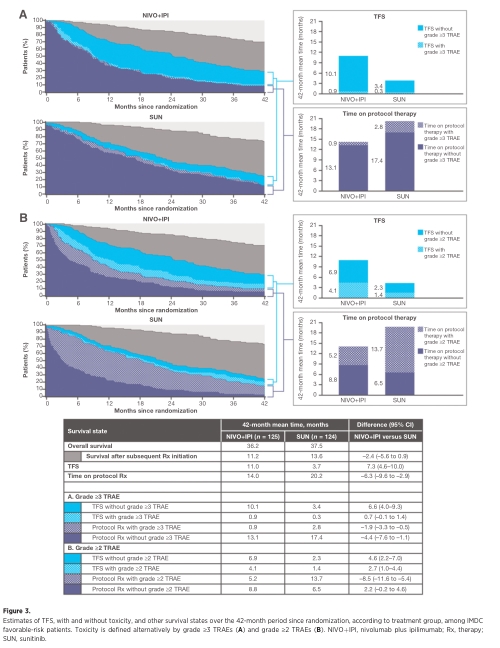
IMDC预后风险良好患者TFS对比
尽管nivolumab + ipilimumab 伴有≥2级TRAE患者较舒尼替尼的平均TFS较长(分别为4.1个月vs. 1.4个月),nivolumab + ipilimumab无毒性患者的平均TFS延长了3倍[6.9个月vs. 2.3个月;差异,4.6个月(95% CI, 2.2 7.0)]。伴有≥3例TRAE的nivolumab + ipilimumab组的TFS为0.9个月,sunitinib组的TFS为0.3个月。

平均TFS汇总
综上,研究表明,晚期肾细胞癌患者(aRCC)一线nivolumab + ipilimumab治疗患者较舒尼替尼治疗获得更长的无治疗生存期(TFS)。
原始出处:
Regan MM, Jegede OA, Mantia CM, Powles T, Werner L, Motzer RJ, Tannir NM, Lee CH, Tomita Y, Voss MH, Plimack ER, Choueiri TK, Rini BI, Hammers HJ, Escudier B, Albiges L, Huo S, Del Tejo V, Stwalley B, Atkins MB, McDermott DF. Treatment-free Survival after Immune Checkpoint Inhibitor Therapy versus Targeted Therapy for Advanced Renal Cell Carcinoma: 42-Month Results of the CheckMate 214 Trial. Clin Cancer Res. 2021 Nov 10. doi: 10.1158/1078-0432.CCR-21-2283. Epub ahead of print. PMID: 34759043.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#细胞癌#
30
学习了
50
#生存期#
46
#晚期肾细胞癌#
31
#停药#
44