CSC&OCC 2015:霍勇:中国心血管病的循证医学研究(2014-2015)
2015-09-14 MedSci MedSci原创
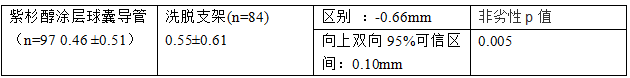
演讲者:北京大学第一医院心血管内科霍勇教授CSPPT研究中国脑卒中一级预防研究(CSPPT)是一项基于中国国情的大规模双盲随机研究。共筛查29190例患者,28202例患者接受依那普利10mg/天*3周,20702例患者进入随机分组,MTHFR CC (n=5513) 、MTHFR CT (n=5513) 、MTHFR TT (n=5513) 。服用依那普利叶酸片10348例患者,服用依那普利
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#血管病#
22
#CSC&OCC#
31
ok
86
#OCC#
27
#循证医学#
26
#循证#
25
#医学研究#
23
#霍勇#
26