NEJM:灼烧样腿痛-病例报道
2020-07-23 MedSci原创 MedSci原创
患者为一名24岁妇女,因严重的灼烧样腿痛2天而到门诊就诊。她既往有先天性感染人类免疫缺陷病毒的病史,为此服用了替诺福韦恩、曲他滨和洛匹那韦-利托那韦。就诊前4天,她还开始每天两次服用麦角胺治疗偏头痛。
患者为一名24岁妇女,因严重的灼烧样腿痛2天而到门诊就诊。她既往有先天性感染人类免疫缺陷病毒的病史,为此服用了替诺福韦恩、曲他滨和洛匹那韦-利托那韦。就诊前4天,她还开始每天两次服用麦角胺治疗偏头痛。
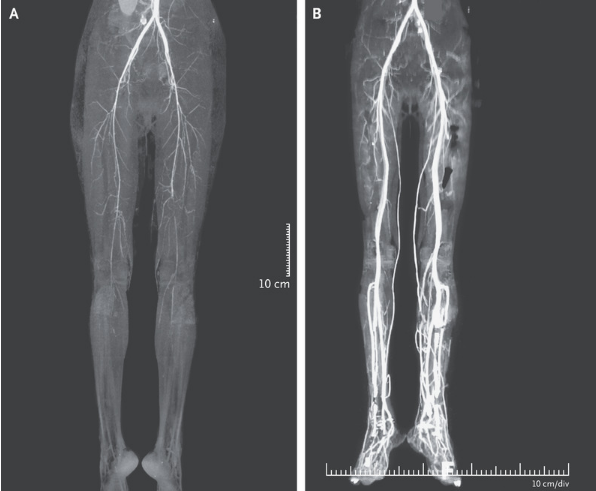
腿部疼痛从脚趾扩展到大腿中部,并伴有脚部变色和行走困难。检查时,双腿均发冷,腘窝和足背脉搏难以触及。计算机断层扫描(CT)血管造影检查发现双腿外动脉下方的动脉弥漫性、对称性管腔狭窄(如图A所示),怀疑为麦角中毒。
利托那韦抑制CYP3A4酶,导致血清麦角胺水平升高,从而引起肢体血管痉挛性缺血。该患者开始接受静脉注射前列腺素和普通肝素治疗。患者疼痛减轻,腿变暖,但由于坏疽,她左侧第二脚趾被截肢。
就诊后2周进行重复CT血管造影发现双腿灌注明显改善(如图B所示)。
原始出处:
Aravind Reghukumar,et al.Burning Pain in the Legs.N Engl J Med 2020;https://www.nejm.org/doi/full/10.1056/NEJMicm1911089
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






长见识了
93
值得关注
92
#不良事件#这是抗病毒🦠药物的少见的不良反应非常值得关注。
0
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
48