NEJM:首次!现货过继性T细胞疗法在临床试验中成功挽救罕见致死性脑感染的癌症患者
2018-10-15 板栗 医麦客
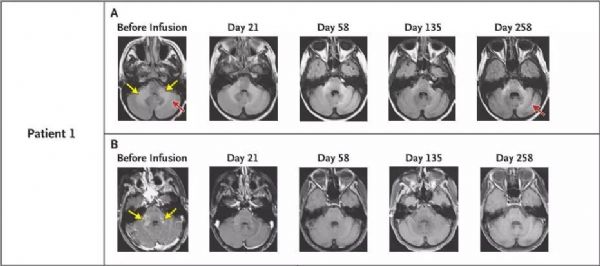
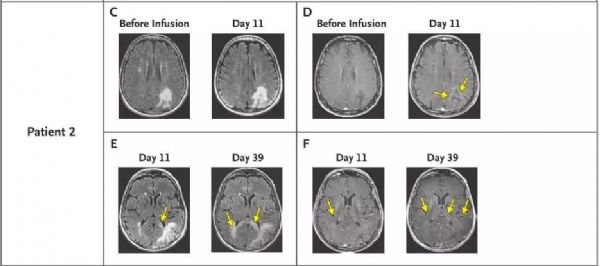
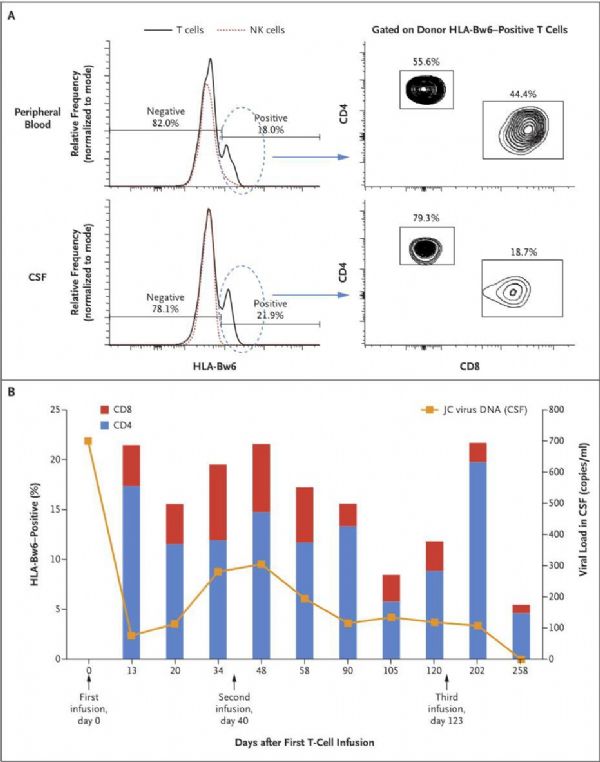
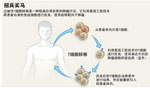
近日,由MD安德森癌症中心干细胞移植和细胞治疗部门的Katy Rezvani教授领导的一项研究显示:3名进行性多灶性白质脑病(PML,通常是致命的)的患者,在接受来自健康供体的活细胞治疗之后,表现出了显着的有效性结果。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#过继性#
45
#过继性T细胞疗法#
40
#癌症患者#
43
#罕见#
41
#T细胞疗法#
47
#致死性#
60
谢谢分享,学习了
53
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
57
谢谢分享,学习了
58