冠脉微血管病变与高血压密切相关,如何治疗?最新共识再添新证据
2022-09-09 心希望快迅 网络
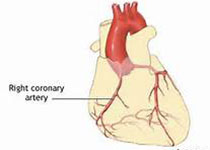
冠状动脉微循环是指由微动脉(< 300 μ m)、心肌组织毛细血管(平均8μm)和微静脉(<500μm)构成的微循环系统。
点击此处查看文中共识:
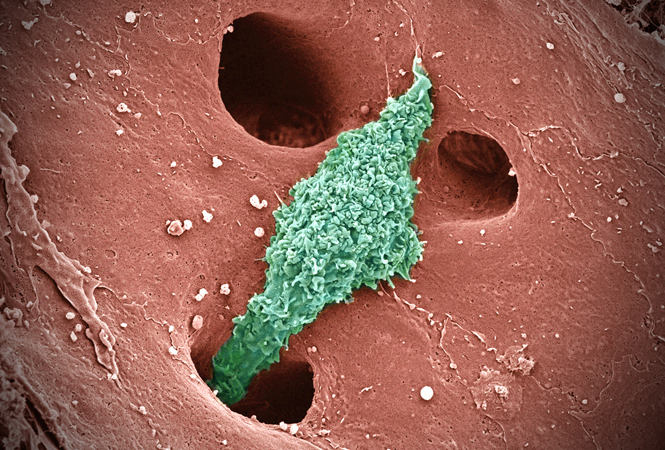
冠状动脉微循环是指由微动脉(< 300 μ m)、心肌组织毛细血管(平均8μm)和微静脉(<500μm)构成的微循环系统。其中微动脉属于肌性动脉,在心外膜下的冠状动脉无固定狭窄时,可显著影响心肌血流灌注,是冠状动脉主要的阻力血管床和心肌代谢场所。其病理机制尚未完全明确,很多研究提示是多因素共同参与的结果,包括动脉粥样硬化、内皮功能失调、炎性反应、微血管舒缩功能障碍、冠状动脉微血管重构等等。
高血压是我国最常见的慢性疾病之一,也是心脑血管疾病最主要的危险因素,成为危害我国国民健康的一大疾病。近些年,高血压动物模型和高血压患者微循环血管减少的现象受到医学界广泛关注和高度重视,发现冠脉微血管病变与高血压密切相关。高血压疾病在我国流行病学形势如何?与冠脉微血管病变存在什么关系?发生冠脉微血管病变之后,该如何治疗?今天,我们做一详细叙述。
01高血压流行病学
高血压患病率和发病率在不同国家、地区或种族之间有差别,工业化国家较发展中国家发病率高。高血压患病率、发病率及血压水平随年龄增长而升高,高血压在老年人中较为常见,尤其是收缩期高血压。我国自20世纪50年代以来进行了4次成年人血压普查,高血压患病率分别为5.11%、7.73%、11.88%、 18.8%,总体上呈明显上升趋势。据估计,我国现有高血压患者2亿以上。但高血压的知晓率、治疗率及控制率均很低,普查资料显示:知晓率为30.2%,治疗率为24.7%,控制率为6.1%。根据2017年我国卫生部心血管病防治研究中心,中国心血管病报道的一项调查报告,城市高血压知晓率、治疗率、控制率和治疗控制率分别为41.1%、35.1%、9.7% 和28.2%;而农村分别为22.5%、17.4%、3.5%和20.4%。如此低的知晓率、治疗率、控制率和治疗控制率,促使我国高血压病致死、致残率居高不下。
02高血压与冠脉微血管
病变密切相关
冠脉微循环包括微动脉(< 300μm)、心肌毛细血管(平均8μm)、和微静脉(< 500μm)。冠脉微循环网是冠脉主要阻力血管床和心肌代谢场所。有研究证实,高血压冠脉储备功能(CFR)减少与冠脉微循环病变和功能障碍有关。
冠状血流储备(CFR)是指冠状动脉最大扩张时血流量与静息状态时血流量的比值,正常值为3~5。它表示冠状循环增加血流量的一种潜在能力。研究表明,高血压患者即使无冠脉狭窄,其冠脉储备也减少30%~50%,且下降程度与高血压左室肥厚程度不一致。高血压时靶器官微血管病变发生于小动脉硬化之前,且在小动脉硬化之后更为严重。病变的微血管是影响靶器官受损的关键血管段。
高血压患者冠脉储备功能降低的主要原因有:
①冠脉阻力增高,主要由微动脉结构和功能改变引起。包括阻力血管重塑,系高血压增加小动脉壁负荷,在多种生长因子作用下,小动脉中层平滑肌和结缔组织重新排列,阻力血管管壁/腔径比值增大,单位心肌组织阻力血管与毛细血管网总横截面积减少,阻力血管内皮功能受损。
②阻力小动脉血管外压力增大,长期高血压致左房压增高,压迫心内膜下冠状动脉,导致心肌灌注不足。左室舒张末压增高,导致舒张期主动脉-左心室压差降低,减少冠状动脉灌注压,这是心肌血流减少和小动脉阻力升高的另一原因。
高血压冠脉微血管病变的临床表现有:
①降压治疗中出现心肌缺血表现,快速降压可以伴发T波倒置;
②微血管性心绞痛,部分高血压患者有心绞痛和心肌缺血心电图表现,但冠脉造影正常,系小冠脉血流储备减低或异常收缩而致心肌缺血,故称“微血管性心绞痛”,属X综合征的一部分,但还不同于X综合征;
③高血压心肌肥厚不伴有冠心病同样可发生心梗、心性猝死、心衰等心血管事件,其主要原因系冠脉阻力血管床病变,微动脉壁/腔比值增大是心脏事件相关最密切指标;
④高血压并存冠心病预后更差,各种心脏事件更易发生且更为严重。
03指南重磅发布,
麝香保心丸疗效确切
中医药在冠心病治疗方面积累了丰富的临床经验,其中,芳香温通类中成药麝香保心丸在长达40余年的临床应用过程中,有效性及安全性得到了广泛认可,积累了大量临床循证证据及实践应用经验。2022年5月10日,中国医师协会中西医结合医师分会心血管病专业委员会联合国家中医心血管病临床医学研究中心在《中国中西医结合杂志》发表了新版的《麝香保心丸治疗冠心病专家共识》,对麝香保心丸的药理作用、临床有效性和安全性进行系统回顾及总结。
据指南介绍,一项荟萃分析共纳入11项RCT共1075例冠脉微血管疾病患者,治疗最短56天,最长1年,与仅使用常规西药治疗相比,联用麝香保心丸可以显著增加冠脉血流储备,降低冠脉微血管阻力指数,升高血清一氧化氮(NO),降低血清C反应蛋白(CRP)。多项研究证实,麝香保心丸单药或与西药联用治疗冠脉微血管疾病患者1~6个月,能有效改善患者临床症状及12导联心电图ST段缺血性下移,对心绞痛后、心肌梗死后、经皮冠状动脉介入术(PCI)术后的微循环障碍及冠脉慢血流均有显著的治疗效果,能显著改善患者冠脉微循环功能,提高相对血流储备分数数值,改善患者的心肌血流灌注。
而且,麝香保心丸的安全性良好,不影响患者肝肾功能、不增加出血风险、与其他药物联用不产生药物相互作用,可长期服用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#血管病#
69
#最新#
46
很受益
48
#微血管#
38
#血管病变#
53
#微血管病变#
45