JAHA:心肌肌钙蛋白诊断慢性肾脏病患者急性心肌梗死的性能
2018-09-25 xing.T MedSci原创
由此可见,通过使用基于肌钙蛋白和肌钙蛋白浓度动态变化的算法,改善了高敏感性心肌肌钙蛋白在疑似NSTE-AMI的CKD患者中的诊断性能。
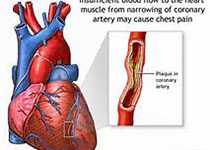
慢性肾脏病(CKD)患者具有较高的心肌梗塞风险。心肌肌钙蛋白是诊断非ST段抬高(NSTE)急性心肌梗死(AMI)首选的生物标志物。在CKD患者中,肌钙蛋白水平通常长期升高,这在疑似NSTE-AMI时降低了它的诊断效用。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章。该研究的目的是推导出一种用于疑似NSTE-AMI的CKD患者一系列肌钙蛋白测量的诊断算法。
研究人员分析了来自前瞻性队列研究中的1494名患者的高敏感肌钙蛋白I(hs-cTnI)测量值和7059名来自临床登记中心的测量了高敏感肌钙蛋白T(hs-cTnT)的患者。前瞻性队列包含280名CKD患者(估计肾小球滤过率<60mL/min/1.73m2)。登记中心数据集包含了1581名CKD患者。
在两个队列中,CKD患者比非CKD患者更有可能被判定为NSTE-AMI患者。hs-cTnI和hs-cTnT用于检测NSTE-AMI的特异性因CKD而降低(hs-cTnI为0.82 vs. 0.91,hs-cTnT为0.26 vs. 0.73),但可通过第一次或3小时后进行第二次测量的优化截止值来恢复。在69%(hs-cTnI)和55%(hs-cTnT)的CKD患者中纳入或排除AMI以及包含连续测量的算法实现了最佳诊断性能。
由此可见,通过使用基于肌钙蛋白和肌钙蛋白浓度动态变化的算法,改善了高敏感性心肌肌钙蛋白在疑似NSTE-AMI的CKD患者中的诊断性能。
原始出处:
Daniel Kraus.et al. Cardiac Troponins for the Diagnosis of Acute Myocardial Infarction in Chronic Kidney Disease.JAHA.2018. https://www.ahajournals.org/doi/full/10.1161/JAHA.117.008032
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#AHA#
30
#心肌肌钙蛋白#
46
#慢性肾脏#
42
好
72