AJH:PD-L1 过表达与 JAK2-V617F 突变负担相关,并与骨髓增殖性肿瘤中的 9p 单亲二体性相关。
2022-01-13 MedSci原创 MedSci原创
PD-L1在MPN细胞中大量表达,包括MPN启动表型定义的CD34+CD45dimCD38−NSC。但靶向 PD-L1 是否可以克服 MPN 中的 NSC 耐药性仍有待在即将进行的研究中阐明。
骨髓增生性肿瘤 (MPN) 是一种慢性干细胞疾病,其特征是骨髓细胞增殖增强、免疫失调和耐药性。JAK2 体细胞突变导致 50-60% 的疾病发生,CALR 突变导致 25-30% 的病例发生。一项研究中,研究人员分析了一个具有良好特征的MPN患者队列中肿瘤细胞中PD-L1的表达,其中有深入的基因组数据。
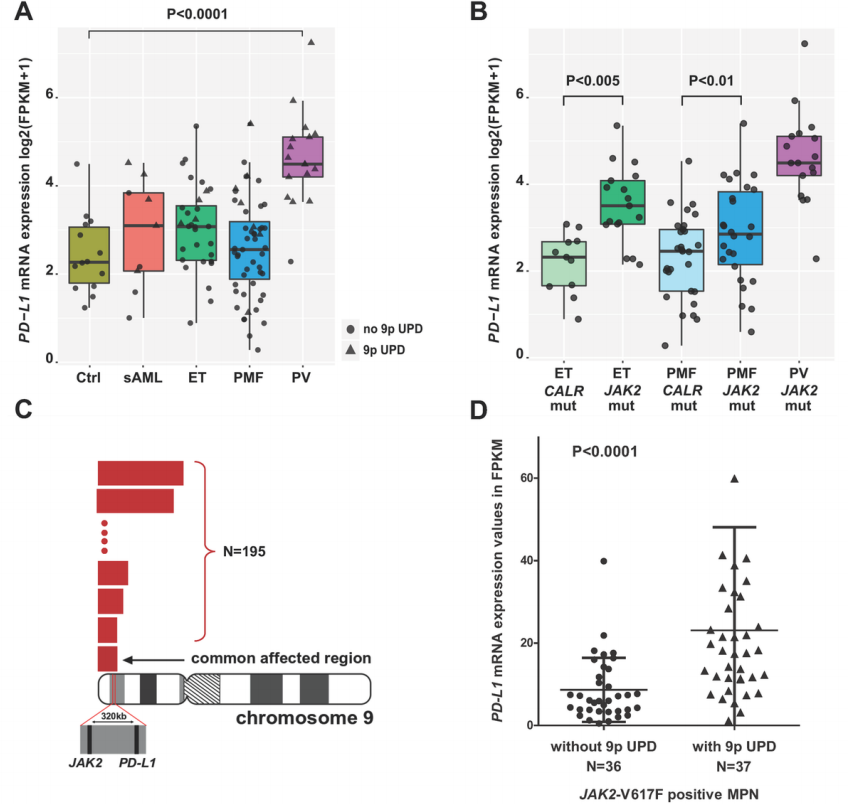
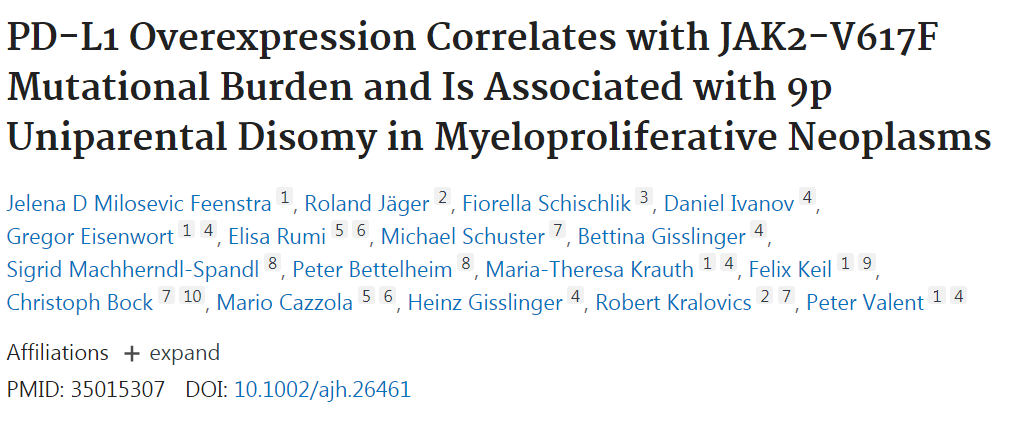
图1:rna测序显示真性红细胞增多症患者髓系细胞中PD-L1表达上调,以及染色体9pUPD在MPN中PD-L1表达上调中的作用。
通过对113例MPN患者的粒细胞进行rna测序,研究人员发现PD-L1的表达在真性红细胞增多症患者中最高,并且PDL1的表达与JAK2-V617F突变负担(R=0.52;P<0.0001)相关。SNP 阵列显示,染色体 9p 单亲二体性 (UPD) 在所有检查的 MPN 患者中均涵盖 PD-L1 和 JAK2。如果存在 9pUPD,则 JAK2-V617F 阳性患者的 MPN 细胞与不存在时相比表达更高水平的 PD-L1(P<0.0001)。
图2:PD-L1位点的种系遗传变异的评价。
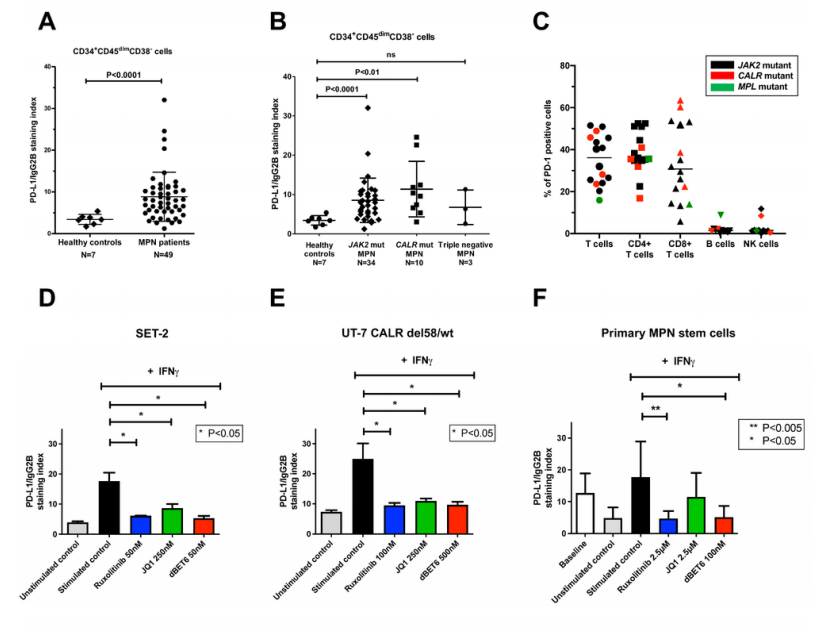
图3:PD-L1在MPN患者骨髓样本中分离的干细胞表面表达上调,鲁索利替尼和dBET6可下调。
此外,基于单倍型的关联分析为 PD-L1 基因座的种系遗传因素提供了证据,这些因素导致 MPN 易感性独立于先前描述的 GGCC 风险单倍型。研究人员还发现,在 JAK2 和 CALR 突变的 MPN 中,PD-L1 在推定的 CD34+ CD38- 疾病起始干细胞 (NSC) 上高度表达。暴露于 JAK2 阻滞剂和 BRD4 靶向剂后,PD-L1 过表达降低,表明 JAK2-STAT5 信号传导和 BRD4 在 PD-L1 表达中的作用。但靶向 PD-L1 是否可以克服 MPN 中的 NSC 耐药性仍有待在即将进行的研究中阐明。
总的来说,研究数据提示PD-L1在MPN细胞中大量表达,包括MPN启动表型定义的CD34+CD45dimCD38−NSC。还证明了PD-L1水平在PV患者的肿瘤细胞中最高,与JAK2-V617F负担和染色体9pUPD相关,并通过BRD4/myc依赖的途径通过IFN-γ暴露促进。研究还提供了第一个证据,表明PD-L1位点的种系遗传因子独立于GGCC(46/1)风险单倍型促进MPN易感性。由于PD-L1是一个主要的耐药性介导的免疫检查点,这些数据可能具有临床意义,并可能为新的PD-L1阻断疗法在MPN中的开发和应用铺平道路。
原始出处:
Milosevic Feenstra JD, Jäger R, Schischlik F, Ivanov D, Eisenwort G, Rumi E, Schuster M, Gisslinger B, Machherndl-Spandl S, Bettelheim P, Krauth MT, Keil F, Bock C, Cazzola M, Gisslinger H, Kralovics R, Valent P. PD-L1 Overexpression Correlates with JAK2-V617F Mutational Burden and Is Associated with 9p Uniparental Disomy in Myeloproliferative Neoplasms. Am J Hematol. 2022 Jan 11. doi: 10.1002/ajh.26461. Epub ahead of print. PMID: 35015307.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#过表达#
35
#突变负担#
31
#JAK#
36
谢谢
60
#PD-L1#
30
#JAK2#
25
#骨髓增殖性肿瘤#
37
好文章,谢谢分享。
60