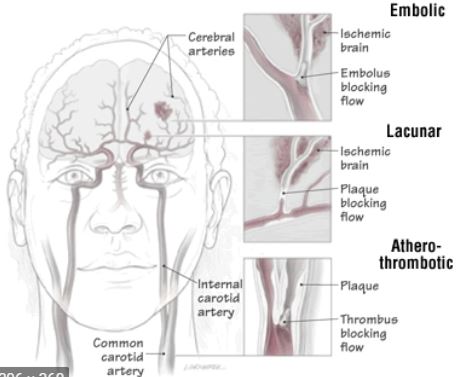
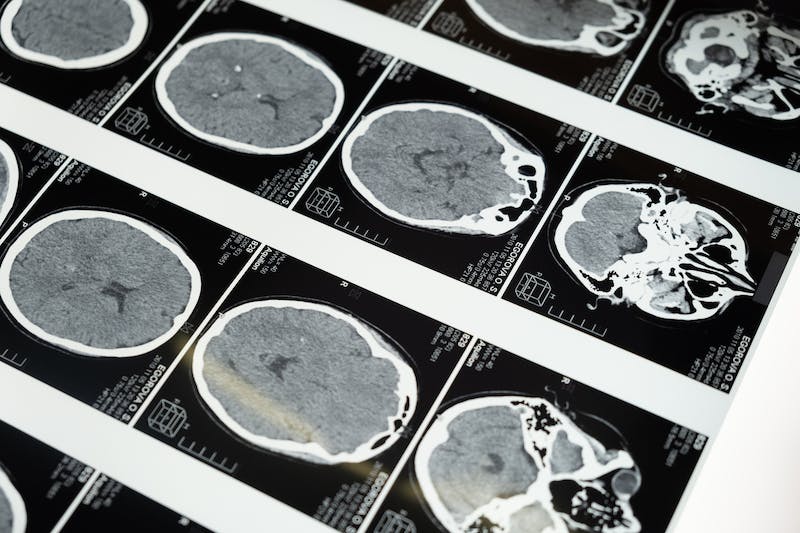
腔隙性脑梗死(LIS)是脑梗死的一大类,主要是指由大型脑动脉的单个穿通支闭塞引起的非皮质性小梗死(直径2-15mm)。这些分支呈锐角起自Willis环的大动脉、大脑中动脉(MCA)主干或基底动脉。
早在1901年,Marie就首次描述了与多发腔隙有关的临床综合征,其特征为可良好康复的突发偏瘫、特征性的小步步态、假性延髓麻痹甚至痴呆。
到20世纪60年代,Fisher提出的详细临床病理学关联产生了所谓的“腔隙性假说”,该假说认为腔隙是由体循环高血压相关的慢性血管病变所致,其可引起多种明确的临床综合征,且通常提示预后良好。
然而,随着CT和MRI的引入,反对“腔隙性状态”的声音越来越多。腔隙性假说的批判者们指出,缺乏腔隙性脑梗死的动物资料或动物模型,且已证实相当一部分腔隙性脑卒中有来源于心脏、主动脉或大动脉的栓子。
那么,头颅磁共振(MRI)检查发现了“腔隙性梗塞”的诊断,需要跟脑梗一样治疗吗?为了确定低剂量与标准剂量静脉注射rt-PA(阿替普酶)对腔隙性与非腔隙性急性缺血性卒中(AIS)的不同疗效和安全性,最近发表在《神经病学》(Neurology)杂志上的研究对ENCHANTED研究进行了事后分析。
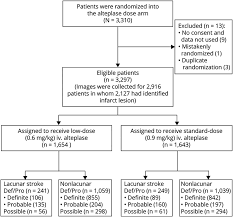
研究人员根据临床和判定的影像学结果,将AIS患者分为LIS与非LIS型AIS(简称AIS)两组。使用逻辑回归模型来确定LIS患者的90天神经功能结局(主要的结局:mRS=2-6;次要结局:其他mRS评分、脑内出血[ICH]和早期神经系统恶化或死亡)。同时,也对低剂量与标准剂量阿替普酶在LIS和AIS组中的治疗效果。
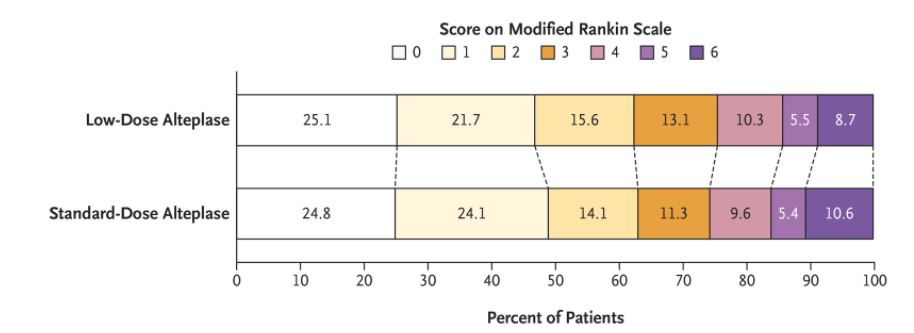
在有影像学和临床数据的2588名参与者中,490名为LIS,2098名为AIS。无论阿替普酶剂量如何,与AIS参与者相比,LIS参与者90天后的神经功能更佳,改善的几率提高40%(mRS 2-6,OR=0.60)。
其中,与标准剂量阿替普酶治疗相比,低剂量阿替普酶治疗对患者功能结果没有影响(OR=1.04 [0.87-1.24]),但可以降低所有参与者的发生ICH风险。低剂量与标准剂量阿替普酶对不同腔隙性和非腔隙性AIS的所有结果没有差异性治疗效果(所有相互作用≥0.07)。
由此可见,从ENCHANTED试验中没有发现证据表明低剂量阿替普酶对急性腔隙性梗死有任何优势。同时,腔隙性梗死也是较之普通脑梗预后更佳的卒中类型。
参考文献:
Zhou Z, et al. Low-Dose vs Standard-Dose Alteplase in Acute Lacunar Ischemic Stroke: The ENCHANTED Trial. Neurology. 2021 Mar 16;96(11):e1512-e1526. doi: 10.1212/WNL.0000000000011598.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Neurol#
33
#腔隙性脑梗塞#
37
好文
62
#脑梗塞#
32
#MRI检查#
42
#脑梗#
23