Cancer Res.: 趋化因子及受体CCL5/CCR5促进乳腺癌转移
2012-06-09 Victor 生物谷
趋化因子CCL5及其受体CCR5在乳腺癌进展过程中的作用一直是个谜。5月25日Cancer Research 杂志在线发表了Marco Velasco-Velazquez等人的研究论文阐明了其中的奥秘。 研究者通过对2254个人乳腺癌标本的微阵列分析发现,在基底型和HER-2亚型的标本中CCL5和CCR5表达升高。表达CCR5的乳腺癌细胞亚群可响应CCL5信号,产生功能性改变。此

趋化因子CCL5及其受体CCR5在乳腺癌进展过程中的作用一直是个谜。5月25日Cancer Research 杂志在线发表了Marco Velasco-Velazquez等人的研究论文阐明了其中的奥秘。
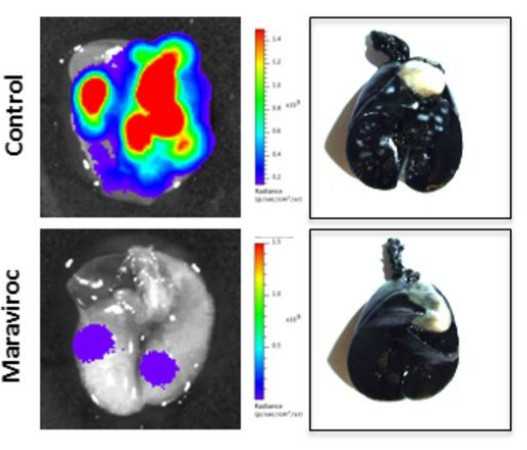
研究者通过对2254个人乳腺癌标本的微阵列分析发现,在基底型和HER-2亚型的标本中CCL5和CCR5表达升高。表达CCR5的乳腺癌细胞亚群可响应CCL5信号,产生功能性改变。此外,癌基因的转化作用诱导CCR5的表达,而且表达功能性CCR5的癌细胞亚群也更具侵袭性。CCR5拮抗剂Maraviroc或者Vicriviroc可降低基底型乳腺癌细胞在体外实验中的侵袭力,但不影响细胞增殖和存活。Maraviroc还可降低小鼠乳腺癌模型中肺转移的几率。
总之,该研究证实了CCL5/CCR5在基底型乳腺癌侵袭力中的作用,并且提示CCR5拮抗剂可作为辅助治疗手段降低该亚型患者肿瘤转移的风险。

doi:10.1016/j.cell.2011.10.017
PMC:
PMID:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Res.:#
32
#趋化因子#
42
#癌转移#
42
#CCL5#
31