Cancer Discovery:CAR-T耐药谁之过?T细胞or癌细胞?
2020-02-03 Blake 转化医学网
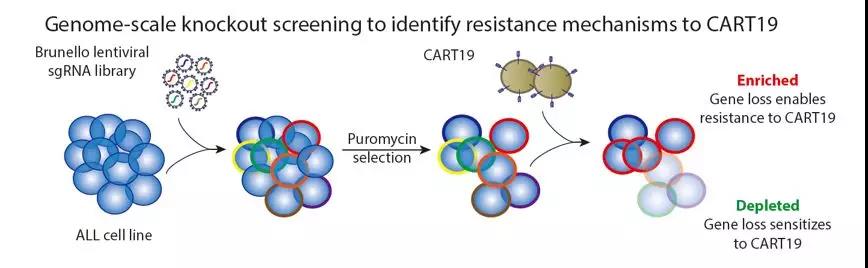
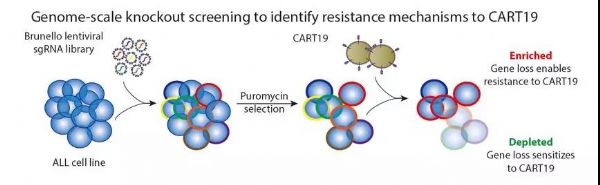
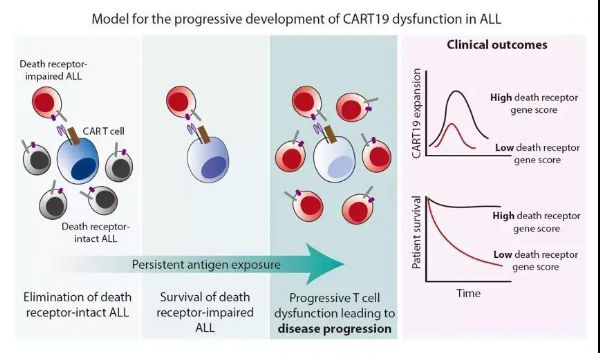
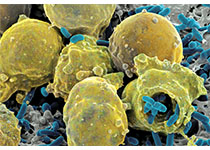
对于B细胞淋巴瘤患者,CART19是一种重要的疗法。然而,其高达10-20%的原发性耐药率是该疗法的一大障碍。但耐药性主要是T细胞导致还是癌细胞导致,尚未定论。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CAR-#
21
#Dis#
33
#cover#
38
#癌细胞#
32
#ISC#
36