Cell:人类肿瘤图谱网络计划分享追踪癌症的策略
2020-04-26 小通 生物通
人类肿瘤图谱网络(Human Tumor Atlas Network,HTAN)计划于2018年9月启动,属于美国国家癌症研究所资助的癌症登月计划的一部分。
人类肿瘤图谱网络(Human Tumor Atlas Network,HTAN)计划于2018年9月启动,属于美国国家癌症研究所资助的癌症登月计划的一部分。
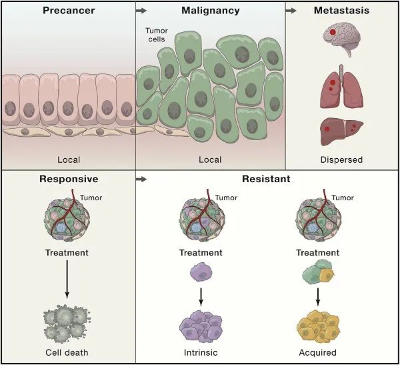
人类肿瘤图谱网络(Human Tumor Atlas Network,HTAN)计划于2018年9月启动,属于美国国家癌症研究所资助的癌症登月计划的一部分。这项计划旨在利用一系列的单细胞图谱来定义人类癌症发展过程中的关键过程和事件,如癌前病变向恶性肿瘤的转化、恶性肿瘤向转移性肿瘤的发展,以及肿瘤对治疗的反应。
近日,Broad研究所、国家癌症研究所、纪念斯隆凯特琳癌症中心等机构的研究人员在《Cell》杂志上概述了人类肿瘤图谱网络研究迄今为止取得的进展。他们认为,这些肿瘤图谱将对人们理解癌症生物学产生深远影响,并有望改善癌症检测、预防和治疗。
这篇文章的通讯作者是单细胞研究领域的大牛、Broad研究所和麻省理工学院的Aviv Regev。她领导的研究团队在文中写道:“之前的工作大多是绘制健康器官的图谱以及在某个时间点对大量癌细胞进行测序,而这项工作形成了很好的补充。”
Regev及其同事计划开展单细胞RNA测序或单核RNA测序,再加上空间信息、外显子组序列、蛋白质组特征、表观基因组数据以及代谢组和微生物组线索,以了解几种成人癌症和小儿癌症的癌前、恶性和转移性癌症样本中的突变、拷贝数变化、表达变化及其他变化。
在这篇文章中,研究团队阐述了这项工作的理由、详细的检测方法以及有望从肿瘤中获得的见解。未来五年,这些研究将在美国的10个跨学科癌症中心开展。例如,费城儿童医院计划将重点放在某些小儿癌症的原发性和耐药性形式上,而其他机构的人员将主要关注原发性、转移性和耐药性的成人肿瘤。
其实,在恶性肿瘤被诊断出来之前,癌症的发展早就有迹可循。因此,研究人员认为,通过分析肿瘤的形态特征、基因组学特征、表观遗传调控因子以及肿瘤微环境,有望弄清癌症发展的详细轨迹。多个研究中心也会将重点放在尚未癌变的样本上。
研究人员称,这项计划还将专注于成熟的肿瘤细胞所产生的细胞,有些细胞对治疗无响应,而有些细胞在最初响应后形成了耐药性。作者表示,HTAN项目将建立一种临床、实验、计算的框架,以便针对各种类型的肿瘤生成信息丰富的三维癌症转化图谱。

他们详细列出了此项技术所使用的工具,包括分子分析、空间分子分析、组织学分析和解剖学分析的工具。有了这些三维的癌症图谱,人们不仅能够更好地了解癌症生物学和治疗策略,还能够利用HTAN数据集来加强癌症的诊断和监控。
研究人员写道:“人类肿瘤图谱网络将提供操作方案、软件和最佳实践指南,以促进各项技术的开发,我们认为这将对人类肿瘤的研究产生深远的影响,包括组织学和组织病理学方面的开放标准。”他们希望这项技术能带来基本资源,以增进对癌症患者的了解、诊断、监测和治疗。
原始出处:Rozenblatt-Rosen O, Regev A, Oberdoerffer P, et al. The Human Tumor Atlas Network: Charting Tumor Transitions across Space and Time at Single-Cell Resolution. Cell. 2020 Apr 16;
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CEL#
25
#Cell#
24
#肿瘤图#
0
#肿瘤图谱#
30
很有意义,谢谢分享
76