JAMA Surgery:对社会经济、伴随疾病因素调整后,乳腺癌患者保乳术和乳房切除术的生存比较:来自瑞典48986例女性乳腺癌患者超6年随访结果
2021-05-20 yd2015 MedSci原创
尽管对很多因素进行了调整,乳腺保乳术(BCS)联合放疗(RT)仍较乳房切除术(Mx)使患者获得生存获益,不管后者是否联合RT。因此,对于同等条件下,MX不应该视等同于BCS。
自从关键研究证实乳腺保乳术(BCS)+术后辅助放疗(RT)跟乳房切除术(Mx)在肿瘤学上是等效的,BCS被推荐用于早期乳腺癌的治疗。即使伴有淋巴结转移,Mx似乎也没有取得明显生存获益。这对于年轻乳腺癌和三阴型乳腺癌(TNBC)也是一样。基于人群的研究发现BCS+RT较Mx术后不进行RT能够带来生存获益。但是,可能有些重要的因素可能导致研究的偏倚。比如,BCS治疗比较少用于社会经济地下的妇女,但是较多用于伴有多发疾病的患者,而且这部分患者进行辅助化疗的比例也比较低。再者,伴随疾病会影响系统和局部治疗的选择以及生存。因此,为进一步详细分析局部治疗跟生存的关系,来自瑞典的团队进行了一项大规模的人群队列研究调查,旨在研究社会经济学地位、伴随疾病跟进行局部治疗的乳腺癌患者的关系。局部治疗分为:BCS 联合RT (BCS+RT), Mx 联合 RT (Mx+RT), 或Mx 不联合 RT (Mx-RT)。

该研究从瑞典国家乳腺癌登记库(NKBC)收集2008年1月1日至2017年12月31日期间诊断浸润性乳腺癌患者,其有明确手术日期、肿瘤大小至多50mm(T1-2)、不多于10个淋巴结阳性(N0-2)以及RT的相关资料。2020年8月19日至2020年11月12日期间进行数据的分析。
研究最终纳入了48986例女性患者,29367例(59.9%)接受BCS+RT治疗, 12413例(25.3%)接受Mx-RT治疗和7206例(14.7%)接受Mx+RT治疗。中位随访时间为6.28年 (范围, 0.01-11.70年)。BCS+RT组较Mx+RT组的肿瘤较小,并且淋巴结阳性较少。而Mx-RT组的淋巴结阳性率跟BCS+RT组的相近。Mx-RT组患者伴有较低的教育水平以及较低的经济收入,而Mx-RT和Mx+RT组较BCS+RT组均伴有较多的伴随疾病。

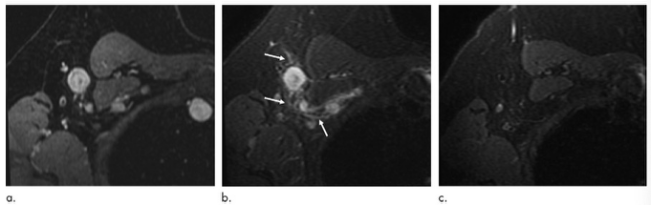
各治疗组的基本信息
随访期间,全因死亡人数为6573,乳腺癌导致死亡为2313例(35.2%)。5年和10年总生存期(OS)和乳腺特异生存期(BCSS)分别为91.1% (OS)和96.3% (BCSS)以及79.5%(OS)和93.1%(BCSS)。未调整分析时,Mx-RT组患者OS最差,而Mx+RT组患者的BCSS最差。
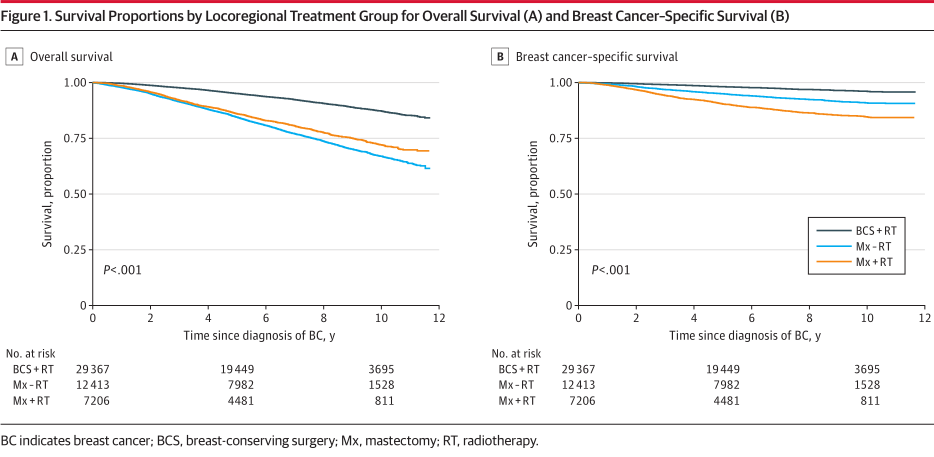
未调整各治疗组的生存比较
按预后组分层分析时,对于明确建议术后辅助RT治疗的患者,比如T1N2和T2N2,Mx-RT治疗的BCSS最差。在所有的预后组中,Mx+RT组的BCSS均较BCS+RT的差。
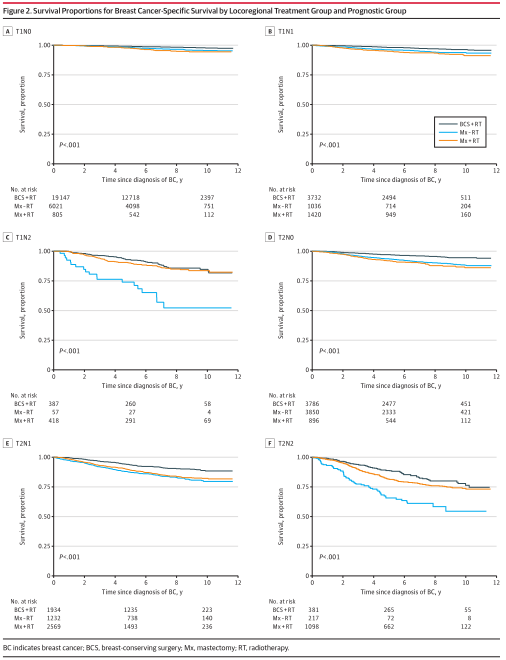
按预后分组比较各组治疗的生存
对诊断年龄、年度以及区域等进行调整时(Model 1),相对于BCS+RT治疗,Mx-RT((OS, HR=1.94, 95%CI (1.82-2.06); BCSS, HR=1.89, 95% (1.69-2.10))和Mx+RT((OS, HR= 2.36, 95%CI (2.21-2.53); BCSS, HR=4.30, 95% (3.88-4.76))均伴有较差的OS和BCSS。在Model 1基础上联合分级、预后分组和分型调整时(Model 2),相对于BCS+RT治疗,Mx-RT((OS, HR=1.91, 95%CI (1.78-2.06); BCSS, HR=1.71, 95% (1.50-1.96))和Mx+RT((OS, HR= 1.24, 95%CI (1.13-1.37); BCSS, HR=1.25, 95% (1.08-1.45))均伴有较差的OS和BCSS。在Model 2基础上联合教育水平、收入水平和出生的国家等调整时(Model 3),相对于BCS+RT治疗,Mx-RT((OS, HR=1.83, 95%CI (1.70-1.97); BCSS, HR=1.67, 95% (1.46-1.91))和Mx+RT((OS, HR= 1.25, 95%CI (1.13-1.38); BCSS, HR=1.25, 95% (1.08-1.46))均伴有较差的OS和BCSS。最后,在Model 3基础上联合伴随疾病等调整时(Model 4),相对于BCS+RT治疗,Mx-RT((OS, HR=1.79, 95%CI (1.66-1.92); BCSS, HR=1.66, 95% (1.45-1.90))和Mx+RT(OS, HR= 1.24, 95%CI (1.13-1.37)); BCSS, HR=1.26, 95% (1.08-1.46))均伴有较差的OS和BCSS。
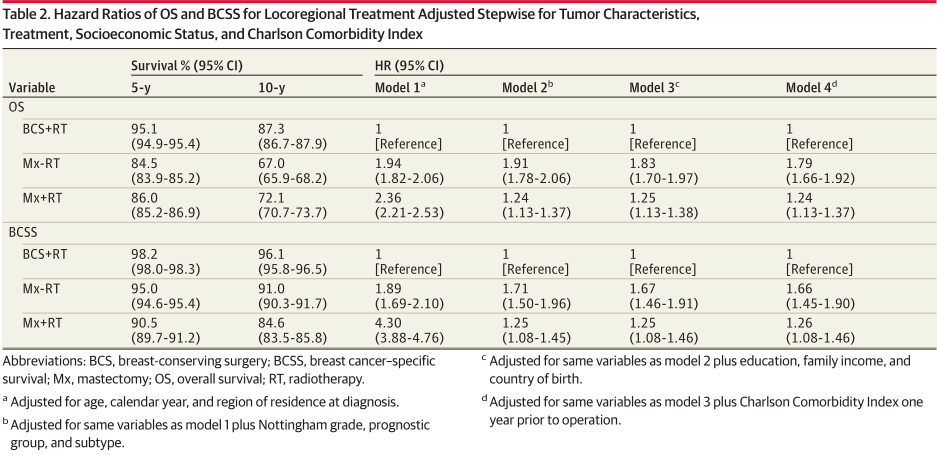
不同调整因素下各组对生存影响比较
综上,尽管对很多因素进行了调整,乳腺保乳术(BCS)联合放疗(RT)仍较乳房切除术(Mx)使患者获得生存获益,不管后者是否联合RT。因此,对于同等条件下,MX不应该视等同于BCS。
原始出处:
Jana de Boniface, Robert Szulkin , and Anna L V Johansson. Survival After Breast Conservation vs Mastectomy Adjusted for Comorbidity and Socioeconomic Status: A Swedish National 6-Year Follow-up of 48 986 Women. JAMA Surg. 2021 May 5. doi: 10.1001/jamasurg.2021.1438. Online ahead of print.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#切除术#
41
#随访结果#
51
#surgery#
47
#社会经济#
42
#GER#
38
#乳腺癌患者#
27
#社会#
33
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
52