Clinical Colorectal Cancer:北京肿瘤医院团队真实世界数据表明瑞戈非尼和呋喹替尼治疗转移性结直肠癌疗效相当
2022-02-18 yd2015 MedSci原创
研究表明,瑞戈非尼和呋喹替尼治疗转移性结直肠癌疗效相当。瑞戈非尼续观呋喹替尼治疗的OS获益更明显,但需要进一步验证。
瑞戈非尼和呋喹替尼在中国均被推荐用于转移性结直肠癌(CRC)患者。但是,目前仍没有头对头研究比较两者治疗转移性结直肠癌患者的疗效。因此,北京肿瘤医院团队开展了回顾性和前瞻性双向研究,比较瑞戈非尼和呋喹替尼治疗转移性结直肠癌的疗效。相关结果发表在Clinical Colorectal Cancer杂志上。
回顾性收集2018年1月至2020年4月期间接受瑞戈非尼或呋喹替尼治疗的转移性CRC患者,并前瞻性的纳入2020年5月至2021年2月期间治疗的患者。主要研究终点为治疗时间失败(TTF),次要结果为总生存期(OS)和不良事件。该研究的另一个目标是探索瑞戈非尼和呋喹替尼治疗的合适顺序。
2018年1月至2021年2月期间,共366名转移性CRC患者接受了瑞戈非尼(n=260)或呋喹替尼(n=106)治疗,其中220例患者为回顾性纳入,146例患者为前瞻性纳入。与呋喹替尼组相比,瑞戈非尼组有更高比例的淋巴结转移。此外,瑞戈非尼组和呋喹替尼组中76.5%和76.4%的患者曾接受过抗VEGF治疗。在RAS和BRAF野生型患者中,瑞戈非尼组54.1%(72/133)和呋喹替尼组59.2%(29/49)接受了抗VEGF治疗。中位随访时间瑞戈非尼组为17.9个月,呋喹替尼组为13.5个月(P=0.392)。
在患者中,70.4%(183/260)和75.5%(80/106)分别接受了单药瑞戈非尼或呋喹替尼(P=0.326)。两组接受局部联合治疗(手术、放疗和介入治疗)的比例相似(10.8% vs 15.1%, p=0.248)。然而,与ICI联合用药在瑞戈非尼组更为常见(17.7%比2.8%,p<0.001),而与化疗联合用药在呋喹替尼组更为常见(4.2%比9.4%,p=0.052)。
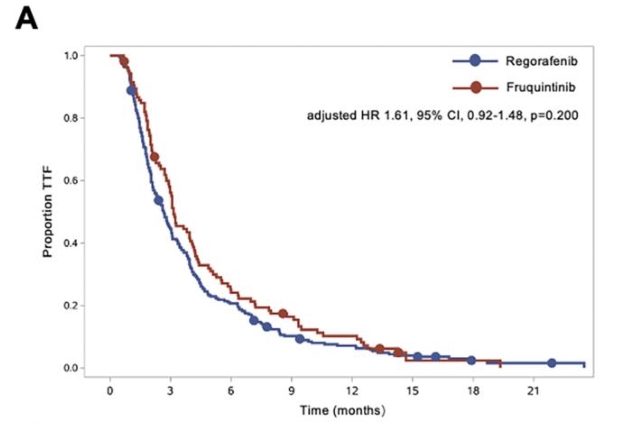
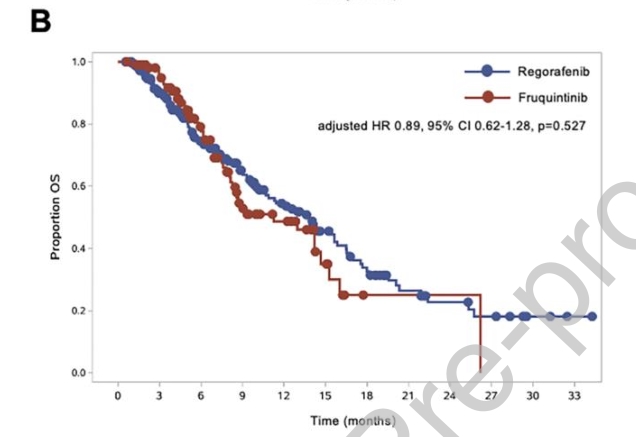
瑞戈非尼组和呋喹替尼组的中位TTF分别为2.7个月(95% CI 2.2-3.0)和3.1个月(95% CI 2.8-4.0)(调整后的HR 1.61, 95% CI, 0.92-1.48, p=0.200)。中位OS分别为13.8个月(95% CI 10.6-15.9)和11.3个月(95% CI 8.1-14.7)(调整后HR 0.89, 95% CI 0.62-1.28, p=0.527)。
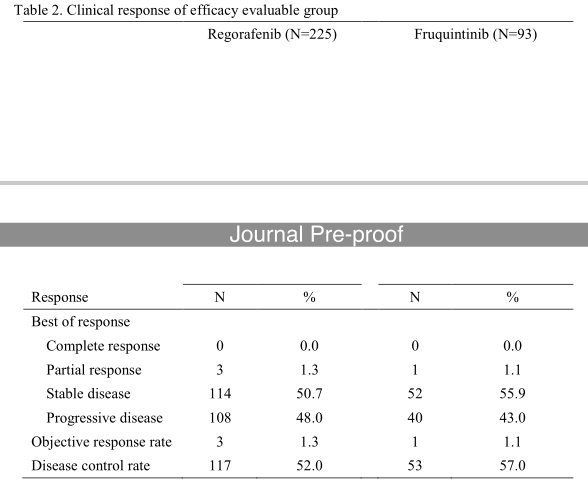
在疗效评价组中,瑞戈非尼组3例患者和呋喹替尼组1例患者达到部分缓解,疾病控制率(DCR)分别为52.0%和57.0%。
亚组分析中,前瞻性组和回顾性组的中位OS结果与整个队列的结果一致。回顾性队列组中,呋喹替尼治疗的中位TTF为3.5个月(95%CI 3.0-5.1),显著长于瑞戈非尼组(2.7个月(95%CI 2.3-3.1))(调整后的HR为1.43,95%CI为1.02-1.99,p=0.037);然而,在前瞻性队列患者中,两治疗组的中位TTF无差异。
在倾向评分分析中,瑞戈非尼组186例患者和呋喹替尼组98例患者进行了匹配,两组间中位TTF (p=0.208)和中位OS (p=0.178)均无显著差异。
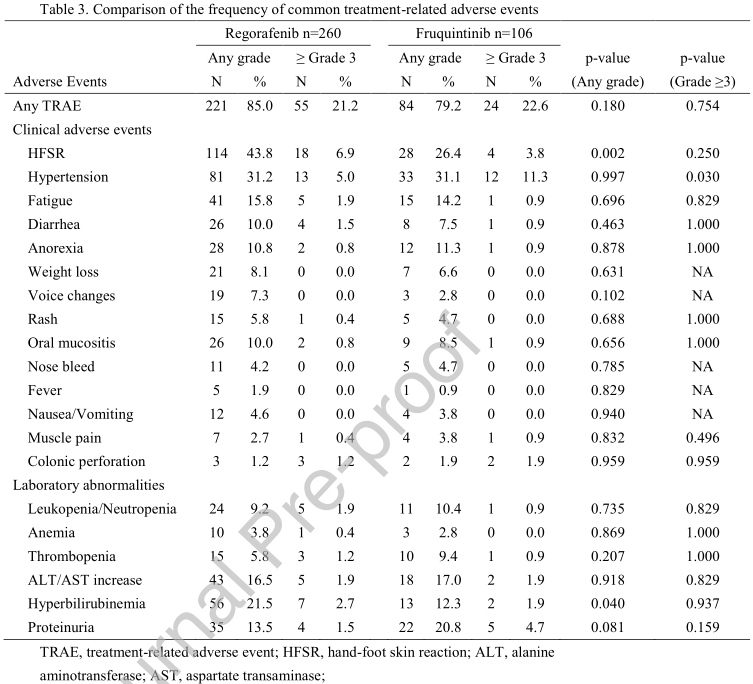
总体而言,瑞戈非尼组85.0%(221/260)的患者发生至少一种AE,,而呋喹替尼组有79.2%(84/106)。其中,瑞戈非尼组和呋喹替尼组分别有8.8%(20/250)和13.0%(13/100)的患者因AE停止治疗。瑞戈非尼组中任何级别的手足皮肤反应(HFSR)和高胆红素血症的发生率显著高于呋喹替尼组(43.8% vs. 26.4%, p=0.002;21.5% vs. 12.3%, p=0.040)。任何级别的蛋白尿在呋喹替尼治疗的患者中更常见(20.8% vs. 13.5%);但结果无统计学意义(p=0.081)。大多数≧3级不良事件在两组之间是相似的,而呋喹替尼组中≧3级高血压发生率较高相关(5.0% vs. 11.3%, p=0.030)。
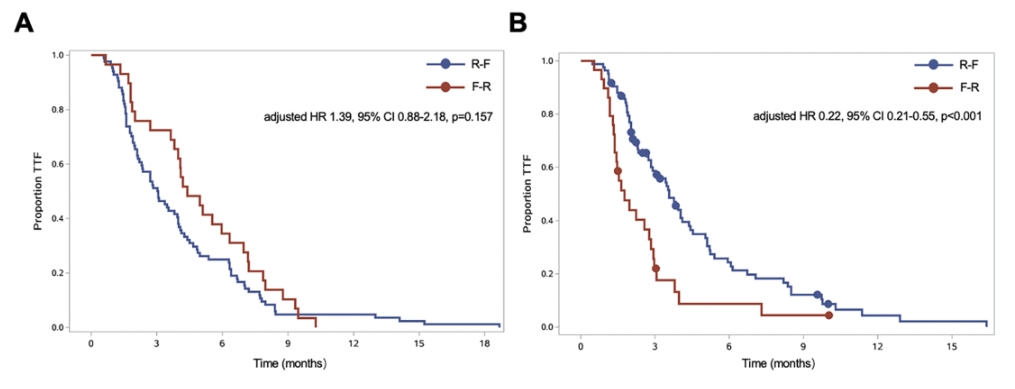
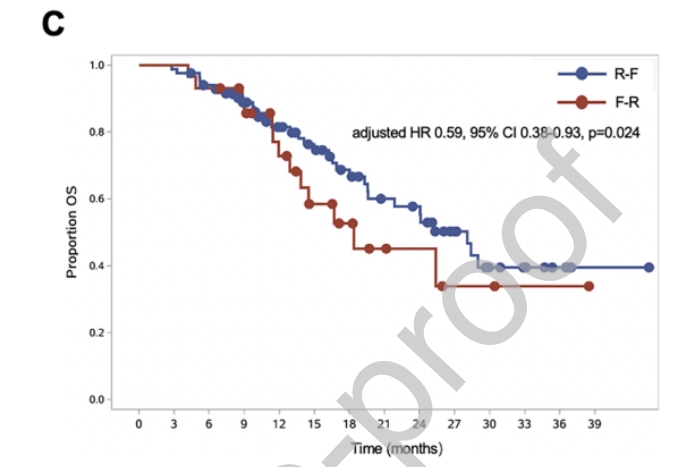
探索最佳治疗顺序时,其中瑞戈非尼续观呋喹替尼治疗组(R-F)有84例,呋喹替尼续观瑞戈非尼治疗组(F-R)有29例。R-F组的中位TTF1为3.1个月(95% CI 2.2-4.0), F-R组的中位TTF1为4.4个月(95% CI 3.6- 6.3)(调整后的HR 1.39, 95% CI 0.88-2.18, p=0.157)。然而,R-F组的中位TTF2[3.6个月(95% CI 2.8-4.4)]显著长于F-R组[1.7个月(95% CI 1.4-2.8)](调整后HR 0.22, 95% CI 0.21-0.55, p<0.001)。从首次入组开始计算的OS(调整后HR 0.59, 95% CI 0.38- 0.93, p=0.024)[28.1个月(95% CI 19.6-NR)比18.4个月(95% CI 12.9-NR)]显示了相同的趋势。
综上,研究表明,瑞戈非尼和呋喹替尼治疗转移性结直肠癌疗效相当。瑞戈非尼续观呋喹替尼治疗的OS获益更明显,但需要进一步验证。
原始出处:
Qi Zhang , Mifen Chen , Zhenghang Wang , Changsong Qi , Yanshuo Cao , Junyan Zhang , Zhi Peng , Xicheng Wang , Ming Lu , Lin Shen , Jian Li , Efficacy and safety comparison of regorafenib and fruquintinib in metastatic colorectal cancer-An observational cohort study in the real world, Clinical Colorectal Cancer (2022), doi:https://doi.org/10.1016/j.clcc.2022.01.007
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#肿瘤医院#
59
#Rectal#
55
#CTA#
52
#真实世界#
50
#转移性#
70
#Colorectal#
38
#结直肠#
47
#clinical#
38