JAHA:乳腺癌患者心脏毒性和心血管生物标志物
2020-11-16 MedSci原创 MedSci原创
NT-proBNP和血红蛋白与接受剂量强化化疗的早期乳腺癌患者的心脏毒性反应显著相关,而高敏心脏肌钙蛋白T则不然。
乳腺癌患者抗癌治疗会受到心脏毒性反应的影响。心脏生物标志物,例如B型利钠肽前体N末端(NT-proBNP)和高敏心肌肌钙蛋白T,可能具有预测价值。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员通过超声心动图、心电图、血液动力学参数、NT-proBNP和高敏心肌肌钙蛋白T对德国乳腺癌组GeparOcto-GBG 84 III期试验中随机分组的853例早期乳腺癌患者进行了评估。患者接受新辅助剂量增强的表柔比星、紫杉醇和环磷酰胺(iddEPC组,n=424)或紫杉醇、非聚乙二醇阿霉素和卡铂(紫杉醇、非聚乙二醇阿霉素、卡铂组,n=429)治疗,共计18周。人类表皮生长受体2阳性的患者(n=354,41.5%)在分配治疗的基础上接受了单克隆抗体治疗。
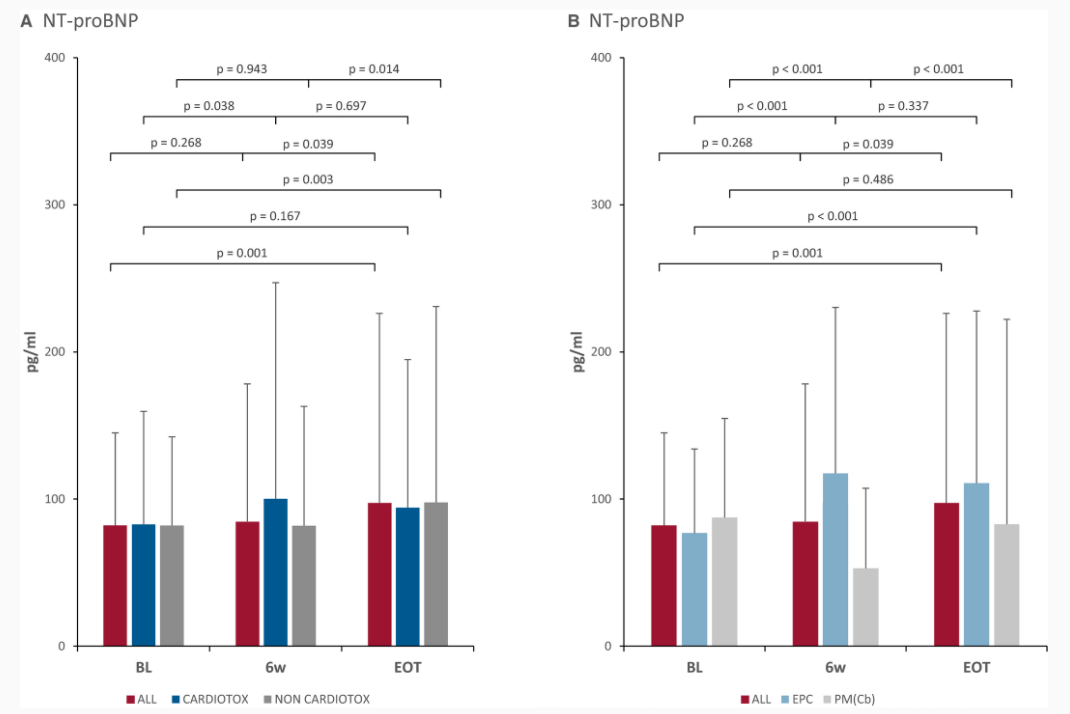
所有患者中有119名患者(12.9%)在治疗期间出现了心脏毒性反应(使用更严格的定义为15名[1.8%])。心脏毒性反应的发生与治疗分组无关(P=0.31)。与心脏NT-proBNP仅在治疗结束时升高的患者相比,伴有心脏毒性反应的患者早期NT-proBNP少量但显著增加(P=0.04)。两组患者的高敏心脏肌钙蛋白T均升高。Logistic回归显示治疗开始6周测量的NT-proBNP(比值比[OR]为1.03; 95%CI为1.008-1.055;P=0.01)和血红蛋白(OR为1.31; 95%CI为1.05-1.63; P=0.02)与心脏毒性反应显著相关。
由此可见,NT-proBNP和血红蛋白与接受剂量强化化疗的早期乳腺癌患者的心脏毒性反应显著相关,而高敏心脏肌钙蛋白T则不然。
原始出处:
Alexandra Maria Rüger.et al.Cardiotoxicity and Cardiovascular Biomarkers in Patients With Breast Cancer: Data From the GeparOcto‐GBG 84 Trial.J AM HEART ASSOC.2020.https://www.ahajournals.org/doi/10.1161/JAHA.120.018143
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#标志物#
30
学习了
78
#AHA#
29
#生物标志#
27
#生物标志#
30
#乳腺癌患者#
36
NT-proBNP和血红蛋白与接受剂量强化化疗的早期乳腺癌患者的心脏毒性反应显著相关,而高敏心脏肌钙蛋白T则不然。
81
对临床有借鉴
83
又了解多一些知识
79