JACC:主动脉瓣重度狭窄只能换瓣吗?来看看这些影响因素!
2021-11-28 MedSci原创 MedSci原创
每5名严重症状的AS患者中就有1名决定不进行干预,这种决定尤其与年龄大和合并疾病有关。
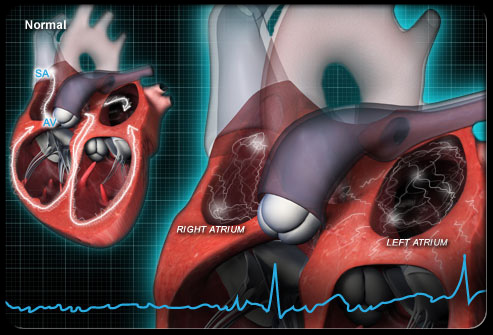
动脉瓣位于左心室和主动脉之间的开口内。主动脉瓣随左心室收缩而开放,以将血液泵入主动脉。如果某种疾病导致瓣叶增厚、僵硬,瓣膜开口会变窄(狭窄)。有时僵硬的瓣膜也不能完全闭合,左心室每次舒张时,主动脉中的血液会通过主动脉瓣漏回心脏(主动脉瓣反流)。
主动脉瓣狭窄时,左心室为了通过狭窄的瓣膜开口将血液泵入主动脉而不得不更加努力地工作,因此左心室的肌肉壁通常会变厚。增厚的心肌需要冠状动脉供应更多的血液,但有时(尤其运动时)血供不能满足心肌的需求。血供不足可导致胸闷、晕厥,有时甚至猝死。心肌也逐渐衰弱,导致心力衰竭。
目前,手术是主动脉瓣狭窄的唯一治疗方法,但指南和实践之间存在着差距。及其,来自法国的研究人员分析了EORP VHDII调查中对严重主动脉瓣狭窄患者进行干预的决定。结果发表在JACC杂志上。

研究人员在2152名严重主动脉瓣患者中,纳入1271名有症状的高梯度主动脉瓣狭窄患者。主要终点是干预的决定。
262名患者(20.6%)作出了不干预的决定。在多变量分析中,决定不干预与年龄较大(每增加10岁,OR=1.34;95%CI:1.11-1.61)、NYHA 分级更低(OR=1.63;95%CI:1. 16-2.30),年龄调整后的Charlson合并症指数较高(OR=1.09;95% CI:1.01-1.17),经主动脉平均梯度较低(每减少10毫米汞柱,OR=0.81;95% CI:0.71-0.92)。
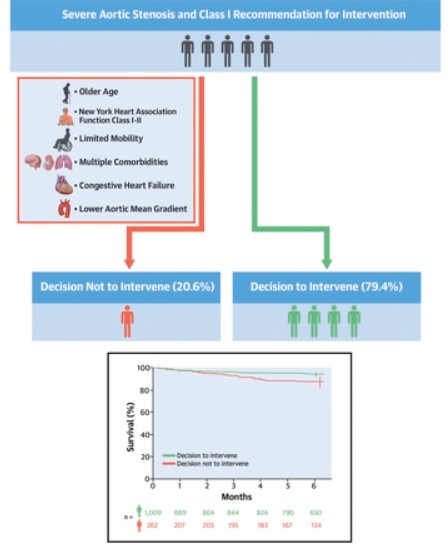
重度症状性主动脉瓣狭窄的当代管理方法
在研究期间,346名患者(40.2%,中位年龄84岁,中位EuroSCORE II(3.1%)接受了经导管干预,515名患者(59.8%,中位年龄69岁,中位EuroSCORE II 1.5%)接受了手术。与选择干预的患者相比,不干预的决定与较低的6个月生存率有关(87.4%;95%CI:82.0-91.3 vs 94.6%;95%CI:92.8-95.9)。
综上,尽管有一级干预建议,但每5名严重症状的AS患者中就有1名决定不进行干预,这种决定尤其与年龄大和合并疾病有关。
参考文献:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#JACC#
47
#ACC#
39
#主动脉瓣#
36
#主动脉#
39
#影响因素#
39