Cell Res:我分泌胰岛素还得肠道菌说了算?中国科学家首次发现,肠道菌的溶解物竟然是胰岛素的通行证
2019-06-30 奇点糕 奇点网
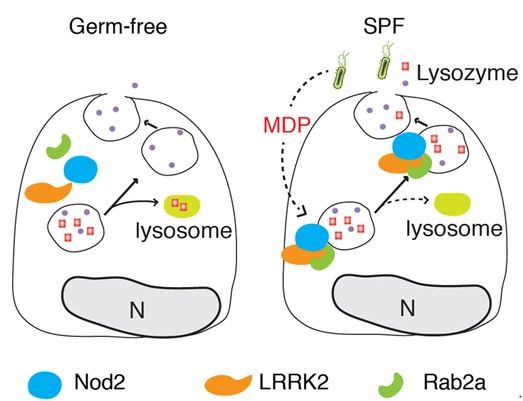
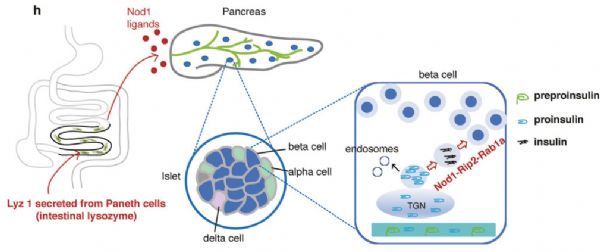
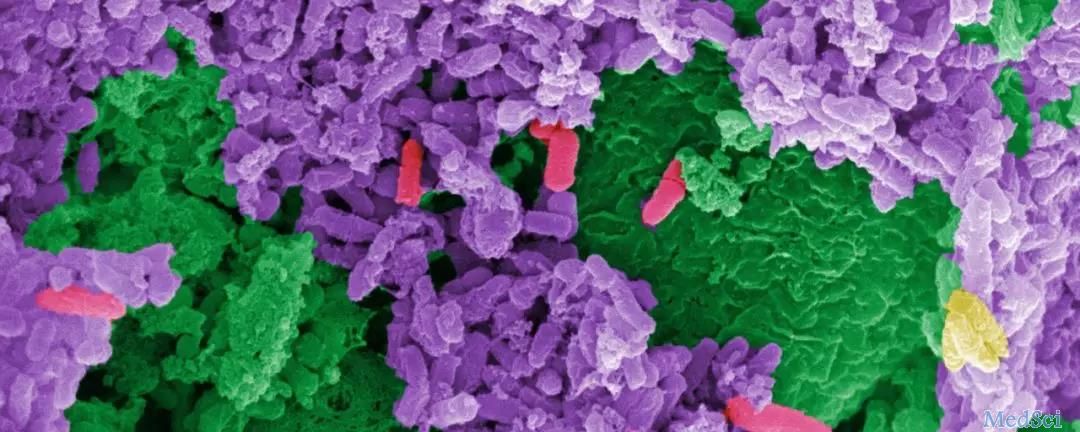
对于分泌胰岛素这么重要的事,竟然要听命于肠道微生物。没有它们,我们可能连胰岛素都分泌不出来……
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cell#
33
#中国科学#
36
#CEL#
29
#分泌#
30
#胰岛#
33
#肠道菌#
29
#中国科学家#
40