J Dental Res:掉了几颗牙?看你健康不
2015-06-09 佚名 生物谷
牙齿提前脱落通常表明一个人口腔疾病的历史。芬兰赫尔辛基大学与国家卫生福利研究院的研究人员在广泛的队列研究结果后,发现牙齿提前脱落与未来心血管事件,糖尿病和死亡有关。缺牙的数目可能作为医生评估慢性疾病风险因素时的一个有用的附加指标。这篇文章发表在Journal of Dental Research。 The National FINRISK 1997研究是以芬兰人口为基础的调查。对8446位年龄在
牙齿提前脱落通常表明一个人口腔疾病的历史。芬兰赫尔辛基大学与国家卫生福利研究院的研究人员在广泛的队列研究结果后,发现牙齿提前脱落与未来心血管事件,糖尿病和死亡有关。缺牙的数目可能作为医生评估慢性疾病风险因素时的一个有用的附加指标。这篇文章发表在Journal of Dental Research。
The National FINRISK 1997研究是以芬兰人口为基础的调查。对8446位年龄在25至75岁的个进行全面的问卷调查,并进行相关临床检查。研究人员以缺牙的数目记录为基线,进行了长达13年对冠心病、急性心肌梗塞、中风和各种原因引起的死亡信息的跟踪,试图找到牙齿掉落与他们之间的统计学联系。
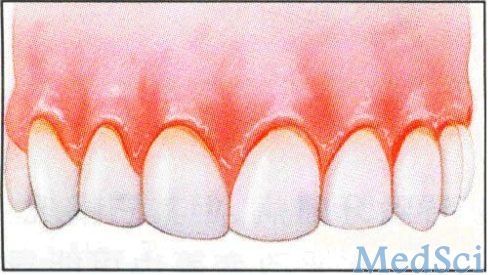
为何进行这项研究?非传染性疾病,如心血管疾病和糖尿病,是世界范围内导致死亡的最常见原因。这几种疾病也知与炎性口腔疾病,如牙周炎有一定关系。牙周炎是牙齿支持组织发生的一种慢性炎症性疾病,临床表现有牙龈出血,增加牙齿的活动性和加深牙周袋,可能会导致牙齿的脱落。如果不进行治疗,牙周炎也是中年和老年人中牙齿脱落的最常见的原因。
根据最后的数据,研究人员分析发现缺牙数目超过五个,冠状动脉心脏疾病事件和心肌梗塞的风险增加了高达140%。缺牙数超过九个以上指向各种疾病风险增加——心血管疾病(51%)、糖尿病(31%)和死亡(37%)。无牙患者相应的风险增加40-68%。传统的危险因素在统计分析过程中也考虑在内。
口腔疾病与全身健康之间的关联最近已经引起人们的重视,世界卫生组织也承认口腔保健在预防致命性的慢性疾病的重要性。牙齿脱落情况,已经被提出替代当前或过去的牙周炎病史作为指示心血管疾病,糖尿病和各种原因死亡率的风险。
原始出处:
J.M. Liljestrand1, A.S. Havulinna2, S. Paju1, S. Männistö2, V. Salomaa2, P.J. Pussinen1.Missing Teeth Predict Incident Cardiovascular Events, Diabetes, and Death.JDR, May 19, 2015.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








好文章,还会关注
60
很好,学习了
118
#dental#
37
看看
131