Clin Chem:免疫富集-偶联MALDI-TOF质谱法直接检测血清中单克隆游离轻链
2019-10-19 gladiator MedSci原创
目前,游离轻链<span lang="EN-US" style="font-size:12.0pt;mso-bidi-font-size:14.0pt;font-family:"Calibri","sans-serif"; mso-fareast-font-family:宋体;mso-bidi-font-family:"Times New Rom
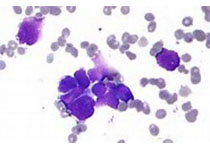
目前,游离轻链(FLC)定量是目前市面上诊断和监测浆细胞疾病(pcd)患者最敏感的血液分析方法。然而,不同于直接检测单克隆FLCs (mFLCs)方法,基于所述к/λFLC比率的量化κ和λ的FLC和判定FLC测定可间接地评估克隆性。通常,异常的FLC比值是PCD的唯一指示,且通过直接方法进行确认可增加诊断的可信度。本研究的目的是开发一种分析灵敏的方法,直接检测mFLCs。
首先比浊FLC定量和免疫固定电泳(IFE)评估了患者血清(N = 167)和对IgG,IgA和总的和游离κ和λ轻链富集,并进行MALDI-TOF MS。这些方法相对于分析灵敏度,用含有mFLCs的连续稀释血清测定这些方法的相对分析灵敏度。
与异常血清方法比率(n = 127),43%单克隆抗体的蛋白质可以经IFE证实, 57%可通过MALDI-TOF MS证实,而不需要FLC富集,87%可经FLC富集MALDI-TOF MS确认。在与正常FLC比血清(N = 40),FLC
MALDI-TOF MS方法鉴定1例mFLC。连续稀释,并通过IFE,比浊法,和FLC
MALDI-TOF MS的含血清的MFLC分析表明,FLC
MALDI-TOF MS分析具有最高的分析灵敏度
研究表明,与MALDI-TOF MS偶联的FLC免疫富集可以直接检测出mFLCs,显著增加了未加FLC富集的IFE和MALDI-TOF MS的异常血清FLC比值的确认,从而为诊断FLC PCDs提供了额外可信度。
原始出处:
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TOF#
41
#克隆#
26
#单克隆游离轻链#
20
#ALD#
33
#质谱#
27