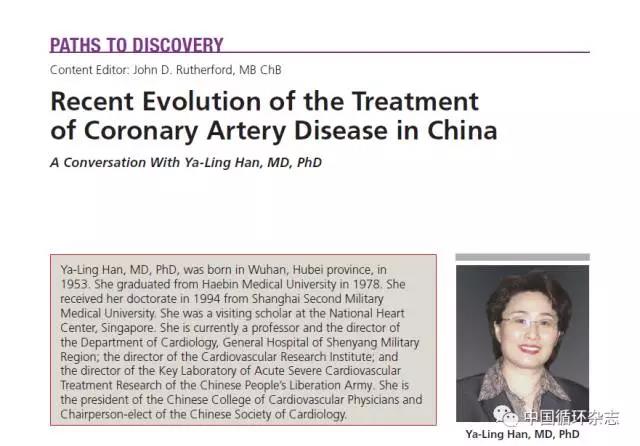
2018长城会(GW-ICC):韩雅玲专题︱比伐芦定在急性心肌梗死中应用的循证之路
2018-10-18 MedSci MedSci原创
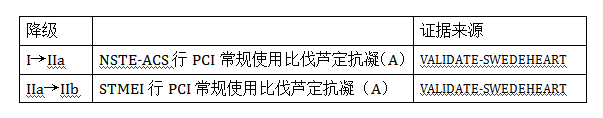
比伐芦定,是一种注射用直接凝血酶抑制剂,具有作用可逆、半衰期短、不引起血小板减少等特点。它可以作用于游离凝血酶,也可以作用于血栓中与纤维蛋白结合的凝血酶。不过,近几年比伐芦定在PCI围手术期的抗凝地位仍受争议。在此次长城会上,韩雅玲院士详细解读了比伐芦定近年来的临床研究新证据,并分享了用药体会。比伐芦定重要临床研究回顾在2004年到2013年期间,比伐芦定的早期临床随机对照研究发现比伐芦定与肝

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#专题#
40
非常不错的临床经验,值得借鉴与推广,学习了,受益匪浅,谢谢分享!
64
#长城会#
37
#循证#
33
#ICC#
34
#韩雅玲#
36
#GW-ICC#
24