ATVB:COVID-19肺炎和社区获得性肺炎患者静脉血栓栓塞风险比较
2020-07-14 MedSci原创 MedSci原创
该研究的结果表明COVID-19肺炎与高凝状态有关。但是,COVID-19肺炎患者的VTE发生率并未明显高于CAP患者。
近日,心血管领域权威杂志Arteriosclerosis, Thrombosis, and Vascular Biology上发表了一篇研究文章,该研究旨在探究和比较新型冠状病毒病2019(COVID-19)肺炎和社区获得性肺炎(CAP)患者静脉血栓栓塞(VTE)的风险和发生率。
研究人员回顾性地分析了2020年1月1日至3月23日期间湖北宜昌市中心人民医院住院的616例肺炎患者的病历。COVID-19肺炎患者在COVID-19定点医院接受治疗,而CAP患者则被送往常规医院接受治疗。研究人员使用帕多瓦预测评分评估了VTE风险。所有患者均接受药物或机械性VTE预防治疗。VTE是通过Duplex超声或计算机断层扫描肺血管造影诊断的。研究人员统计并比较了COVID-19和CAP组之间的差异。所有统计检验均为双侧检验,P<0.05被认为具有统计学意义。
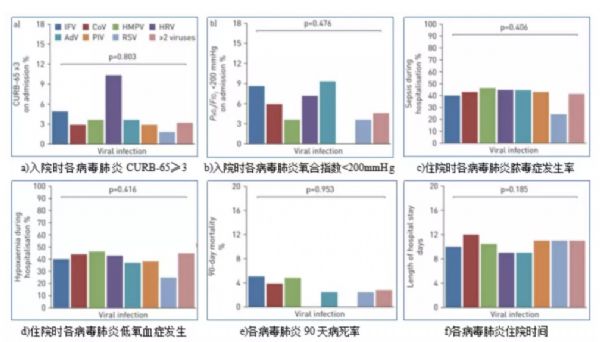
在616名患者中,有256名患有COVID-19肺炎,有360名患有CAP。COVID-19肺炎组的VTE总发生率为2%和CAP组为3.6%(P=0.229)。15.6%的COVID-19肺炎患者和10%的CAP患者被归类为VTE高风险(Padua评分>4),差异显著(P=0.036)。在那些高危患者中,COVID-19肺炎组的VTE发生率为12.5%,CAP组的VTE发生率为16.7%(P=0.606)。重症患者的亚组分析显示,COVID-19组的VTE率为6.7%,而CAP组为13%(P=0.484)。COVID-19组和CAP组的院内死亡率分别为6.3%和3.9%(P=0.180)。
该研究的结果表明COVID-19肺炎与高凝状态有关。但是,COVID-19肺炎患者的VTE发生率并未明显高于CAP患者。
原始出处:
Fei Mei.et al.Comparison of Venous Thromboembolism Risks Between COVID-19 Pneumonia and Community-Acquired Pneumonia Patients.ATVB.2020.https://www.ahajournals.org/doi/10.1161/ATVBAHA.120.314779
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#静脉血栓栓塞风险#
48
#获得性#
35
#风险比#
43
#TVB#
38
#静脉#
28
#静脉血#
28
学习
93
#社区#
29