Journal of Neurology, Neurosurgery & Psychiatry:神经炎症预示进行性核上麻痹的疾病进展
2021-06-23 MedSci原创 MedSci原创
小胶质细胞激活的PET分子成像和tau病理可以预测PSP的临床进展。这些数据鼓励了对免疫调节方法的评估,以治疗疾病的PSP和潜在的PET分层患者在早期临床试验。
进行性核上麻痹(PSP)除了tau病理和神经元丧失外,还会发生神经炎症。然而,体内成像标记物对PSP中这些过程的预后价值仍不清楚。
Journal of Neurology, Neurosurgery & Psychiatry杂志最近发表研究论文,检验了皮质下神经炎症的基线体内成像评估可以预测PSP患者的临床进展这一主要假设。

该研究的主要假设是,与PSP病理相关的皮质下区域的炎症促进了疾病的进展。测试了神经炎症的体内基线测量([11C]PK11195 PET)是否可以预测PSP-Richardson综合征患者的年临床进展率。测试了关于基线皮质炎症、tau病理([18F]AV-1451 PET)和区域脑容量(结构MRI)的预测价值的次级假设。
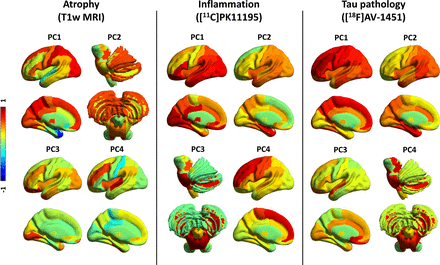
灰质体积,炎症和tau病理的主成分(PCs)。灰质体积的前四个PCs(左图),[11C]PK11195 BPND(中间图)和[18F]AV-1451 BPND(右图)。颜色代表每个组件的大脑区域的roated重量(范围:从−1到1)。
17例PSP-Richardson综合征患者接受了基线多模态成像评估,包括[11C]PK11195正电子发射断层扫描(PET)以指示小胶质细胞活化,[18F]AV-1451 PET用于tau病理和结构MRI。用进行性核上麻痹评分量表(PSPRS)(平均间隔5个月)在基线和连续4年测量疾病的严重程度。
用三主成分分析(PCA)总结了区域灰质体积和PET配体结合潜力。纵向PSPRS评分采用线性混合效应模型。单模态成像预测因子与个体估计的进展率进行回归,以确定基线成像标记物的预后价值。
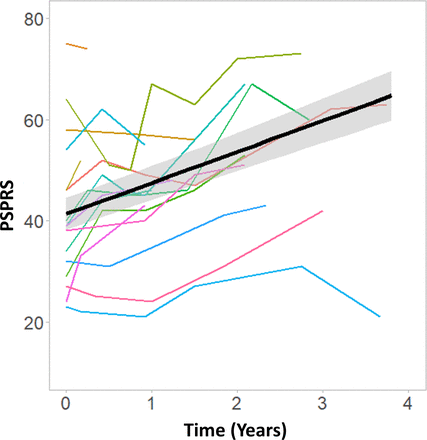
PSPRS随时间变化的临床严重程度。彩色线表示个体患者PSPRS评分的时间进程。黑线表示组级的线性拟合。
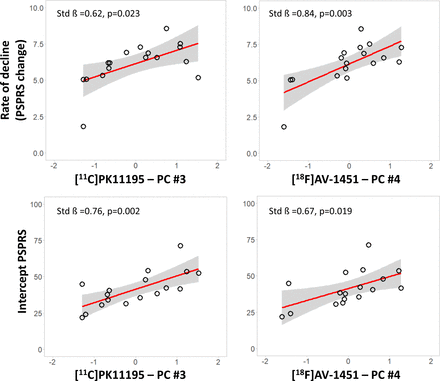
炎症和tau PET标记物与临床严重程度和进展相关。PSPRS分数(上行)和截距PSPRS分数(下行)对每种特异性主成分(经协变量修正的X轴残差分量值)的基线分数的年度变化的显著回归分析:[11C]PK11195 PET(左面板)和[18F]AV-1451 PET(右面板)。以年龄、教育程度和性别为协变量,报告了每种模型的估计参数。
反映脑干和小脑神经炎症和tau蛋白负担的PCA成分与PSPRS随后的年变化率相关。神经炎症和tau病理的PCA衍生PET标记物与同一区域的区域脑容量相关。然而,仅MRI体积并不能预测临床进展的速率。
该研究的主要发现是,皮质下神经炎症与基线PSP的临床严重程度,并与更快的后续临床进展相关。在皮层下tau病理评估中也发现了类似的效应,与PSP中[18F]AV1451结合的解释相关。PET标记物彼此相关,并与同一区域萎缩的结构性MRI测量相关联。然而,皮层下灰质体积与随后的临床进展不相关,也与基线时的临床严重程度不显著相关。同样,基线时的临床严重程度并不能预测接下来几年的临床进展,这表明在疾病的不同阶段,临床变化的年速率大约是恒定的。
总之,该研究结果支持神经炎症与PSP-Richardson综合征进展的相关性。[11C]PK11195可能是PSP临床试验的一个有价值的生物标志物,可以作为结构性MRI的补充。PET标记物可用于基于预后的患者分层和治疗反应的评估,支持PSP疾病改善治疗的免疫调节策略(,单独或联合针对tau蛋白和其他致病途径的治疗)的发展。
原文出处
Malpetti M, Passamonti L, Jones PS, et al.Neuroinflammation predicts disease progression in progressive supranuclear palsy. Journal of Neurology, Neurosurgery & Psychiatry 2021;92:769-775. https://jnnp.bmj.com/content/92/7/769
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#神经炎#
48
#进行性#
41
#Psychiatry#
47
#GER#
38
#Neurol#
38
#surgery#
48
#疾病进展#
34
#ROS#
41