第34届欧洲泌尿外科学会(EAU)大会:Atezolizumab对晚期转移性泌尿道癌有效
2019-03-21 不详 网络
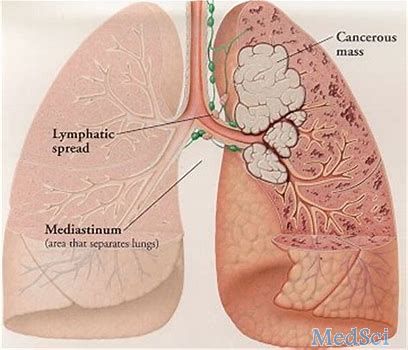
根据第34届欧洲泌尿外科学会(EAU)大会上发表的一项研究,Atezolizumab对局部晚期或转移性尿路上皮或非尿路上皮癌患者的治疗具有耐受性和有效性。
根据第34届欧洲泌尿外科学会(EAU)大会上发表的一项研究,Atezolizumab对局部晚期或转移性尿路上皮或非尿路上皮癌患者的治疗具有耐受性和有效性。
前瞻性、开放标签、单臂SAUL试验研究了997名局部晚期或转移性泌尿道癌患者(中位年龄68岁)。在这些患者中,10%的患者的ECOG表现状态为2,61%的患者有1个或更多的转移性疾病。所有患者每3周静脉注射1200mg Atezolizumab,直至失去临床获益或不可接受的毒性。结果表明,在意向治疗人群中,中位总生存期为8.7个月,在12个月时仍有41%的存活率,中位无进展生存期为2.2个月。3%的患者对治疗作出完全反应,11%的患者对治疗作出部分反应,疾病控制率为40%。
原始出处:
http://www.firstwordpharma.com/node/1630691#axzz5ioDx2kLe
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#EAU#
38
#mAb#
41
#尿道#
43
#欧洲#
42
#尿道癌#
38
#转移性#
33