Cell Metabolism:食品中广泛使用的诱惑红和落日黄,会诱导和加速结肠炎发展!
2021-05-18 生物世界 生物世界
近日,来自美国纽约西奈山伊坎医学院的研究人员在《Cell Metabolism》上发表了题为Food colorants metabolized by commensal bacteria promo
炎症性肠病(IBD)是涉及到不同肠道的一种慢性炎症疾病,患者会出现长期的腹泻、腹痛,甚至血便,随着发病率的上升,已成为了我国常见的消化系统疾病。对该疾病病因的长期研究表明,遗传易感性和环境因素似乎都影响着IBD的发展。虽然白介素23(IL-23)已被明确可能是最有助于IBD发展的免疫因子之一,但导致疾病的环境因素仍让人难以捉摸。
近日,来自美国纽约西奈山伊坎医学院的研究人员在《Cell Metabolism》上发表了题为 Food colorants metabolized by commensal bacteria promote colitis in mice with dysregulated expression of interleukin-23 的研究成果,发现在IL-23表达失调的情况下,诱惑红和日落黄等特定的食用色素会诱导和加速结肠炎的发展,是影响IBD的新型环境危险因素。
前期实验中,研究人员发现,在正常饮食饲喂时,他莫昔芬(TAM)诱导的IL-23过表达R23FR小鼠似乎并不会发生结肠炎,而当其周期重复性食用定制饮食后,结肠炎便会发病。在对喂养R23FR小鼠的饮食中的不同成分筛选后,研究人员发现了一种成分食用色素-诱惑红,或许这是诱导结肠炎发生的原因。
为了测试诱惑红是否会促进诱发结肠炎,研究人员分别对IL-23过表达R23FR小鼠喂食了含诱惑红的TAM饮食和不含任何着色剂的TAM饮食,与之前的结果一致,喂养含诱惑红的TAM饮食的老鼠经历了与人溃疡性肠炎相似的结肠炎发病周期,即发病期,恢复期和复发期。这也表明,诱惑红能够诱导结肠炎的发展。
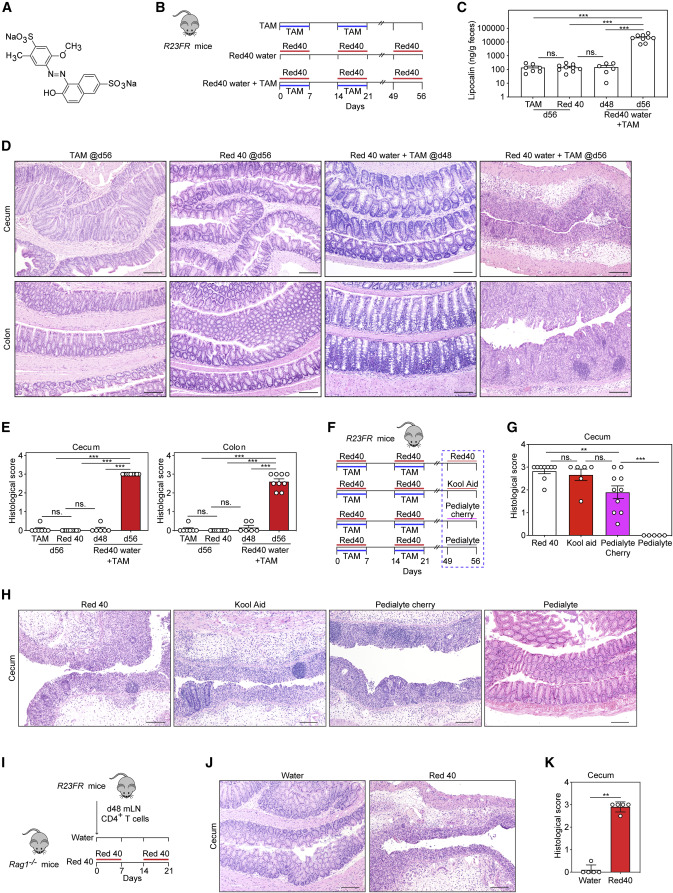
诱惑红(red 40)诱导过表达IL-23小鼠的结肠炎
诱惑红作为被广泛添加至食品、饮料和药品中的可食用色素,已经测试证明其对细胞并没有毒性、致癌或诱变作用。研究人员猜测,它之所以不会诱使大规模人群发生结肠炎,可能是由于其免疫耐受性的提高。因此,研究人员测试了诱惑红处理的对照小鼠的调节性T细胞是否能抑制或减轻结肠炎的发展,结果发现正常小鼠在IL-23过表达之前暴露于诱惑红中,会使得小鼠中出现由调节性T细胞介导的对该色素的耐受性,而IL-23表达的升高会阻止对该化合物的耐受性,促进结肠炎的发展。对导致结肠炎发展的免疫致病机制进一步研究后,发现IL-23过表达促进的CD4+T细胞产生的IFN-γ是诱使和加快结肠炎发展主要细胞因子。
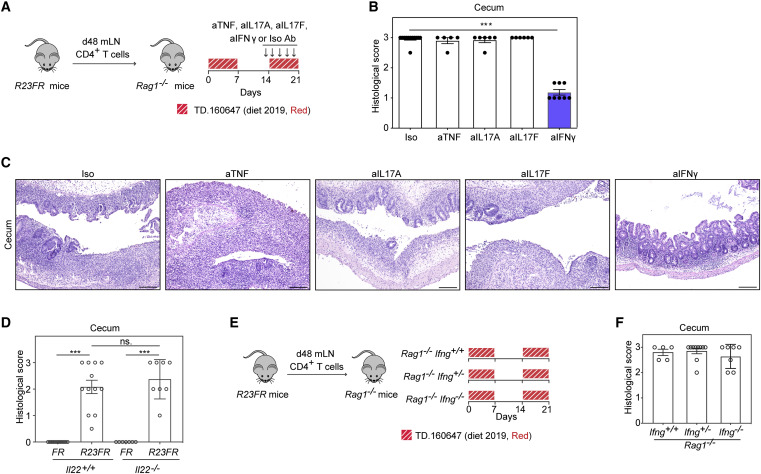
产生IFN-γ的CD4 + T细胞对于盲肠炎症的发展至关重要
之后,研究人员对与诱惑红促肠炎的致菌机制进行了分析,其通过16S rRNA测序测试了诱惑红诱导的结肠炎是否由微生物参与介导。结果发现,诱惑红引起结肠炎的能力取决于微生物菌群的种类,拟杆菌属的卵形拟杆菌和链球菌属的粪肠球菌等共生菌可能有助于诱惑红诱发并促进小鼠结肠炎的发展。
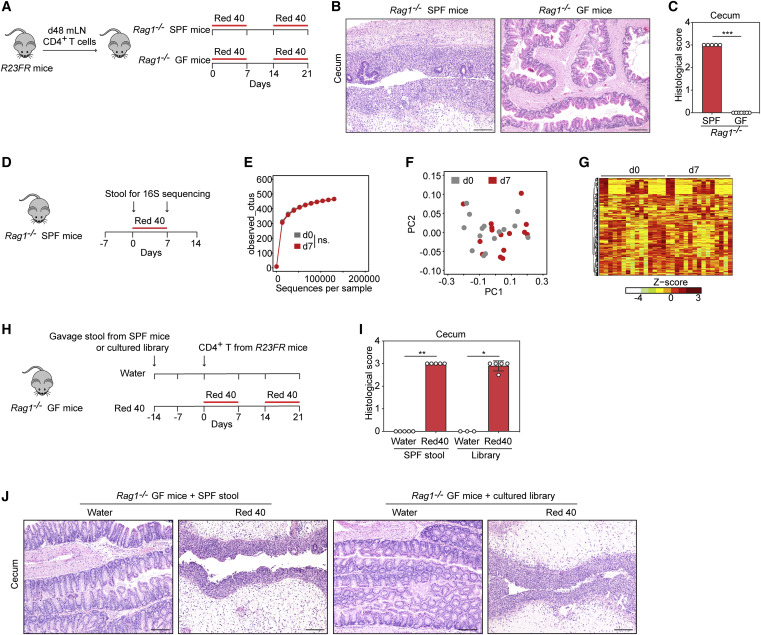
诱惑红诱导的结肠炎取决于肠道菌群
诱惑红可通过在胃肠道中进行偶氮还原而代谢为两种主要代谢物:4-氨基磺酸甲酚钠(CSA-Na)和1-氨基-2-萘酚-6-磺酸钠(ANSA-Na)。那么其对结肠炎的促进作用是否与代谢物也有关呢?进一步的实验表明, ANSA-Na确实对于小鼠结肠炎的诱发具有促进作用,而CSA-Na并不参与其中。研究人员还发现,同样可经偶氮还原产生的ANSA-Na的另一种广泛使用的色素日落黄也具有相同的促结肠炎作用。
简而言之,研究人员发现了世界上最广泛使用的偶氮染料诱惑红(Red 40)和日落黄(Yellow 6)在IL-23高度表达的情况下,具有诱发结肠炎的风险,也会促进结肠炎发展,是值得我们关注的新的影响健康的危险因素!
原始出处:
Zhengxiang He, Lili Chen, Jovani Catalan-Dibene, et al. Food colorants metabolized by commensal bacteria promote colitis in mice with dysregulated expression of interleukin-23. Cell Metabolism, 2021. DOI:https://doi.org/10.1016/j.cmet.2021.04.015.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Cell#
34
#Meta#
28
#MET#
32
#CEL#
23
#Metabolism#
30
#ABO#
29