Gut:基于粪便免疫化学试验的结直肠癌筛查项目长期性能如何?
2017-11-04 xing.T MedSci原创
由此可见,重复的FIT筛查可显著减轻结直肠疾病的负担,促进结肠镜检查资源的有效利用。五轮FIT试验累积检出率与结肠镜检查的初级筛查相似,这一结果支持在评估试验效能时考虑到重复FIT的累积敏感性。
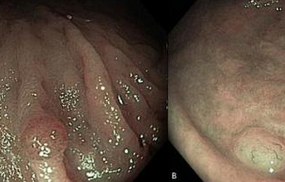
基于2年粪便免疫化学试验(FIT)的结直肠癌(CRC)筛查项目长期性能仍不明确。近日,消化病领域权威杂志Gut上针对这一问题发表了一篇研究文章。
在50岁到69岁的个体组成的样本采用FIT(OC透析乳胶凝集试验;临界值为20 µg血红蛋白/g粪便)进行反复筛查,研究人员评估了:(1)在每一轮的筛查中,FIT试验的阳性率、CRC和晚期腺瘤的检出率以及FIT试验对晚期肿瘤的阳性预测值(PPV),(2)经过五轮FIT试验累计CRC和晚期腺瘤的检出率。
在12年间(2002年-2014年),123347名参与者进行了高达六次的FIT筛查,其中781例CRCs和4713例晚期腺瘤患者被诊断。从第一轮到第三轮(率比(RR)为0.25,95%可信区间为 0.20-0.32)和到第二轮(RR为0.51,95%可信区间为0.47-0.56 ),CRC和晚期腺瘤检出率大幅下降轮,然后保持稳定。在第二轮筛查中,晚期肿瘤的PPV下降了18%(RR为0.82,95%可信区间为0.77-0.89),没有进一步的降低,由于FIT的阳性率随之下降(从第一轮至第六轮FIT的RR为0.56,95%可信区间为0.53-0.60)。连续五轮筛查累积的CRC和晚期腺瘤的检出率分别为8.5‰(95%可信区间为7.8-9.2)和58.9‰(95%可信区间为56.9-61)。
由此可见,重复的FIT筛查可显著减轻结直肠疾病的负担,促进结肠镜检查资源的有效利用。五轮FIT试验累积检出率与结肠镜检查的初级筛查相似,这一结果支持在评估试验效能时考虑到重复FIT的累积敏感性。
原始出处:
Manuel Zorzi,et al. Long-term performance of colorectal cancer screening programmes based on the faecal immunochemical test. Gut. 2017. http://dx.doi.org/10.1136/gutjnl-2017-314753
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








不错的研究
64
#筛查项目#
30
#粪便免疫化学试验#
37
学习了谢谢了
50
学习学习.继续关注
48
#结直肠#
27
#粪便#
30