Circulation:动力相关蛋白1的结合伴侣MiDs参与有丝分裂调控,在肺动脉高压的病理过程中发挥重要作用
2018-07-23 MedSci MedSci原创
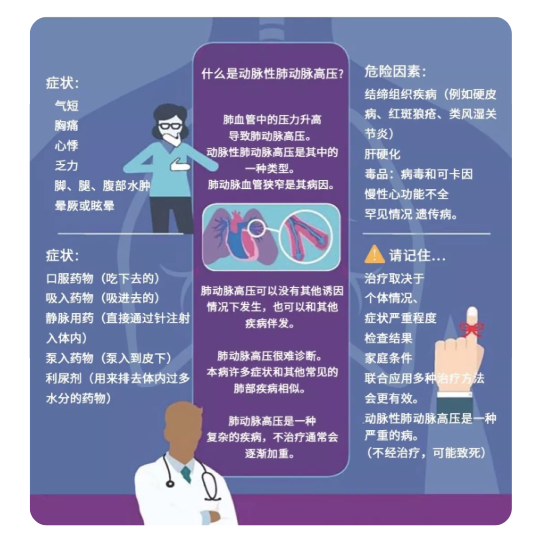
肺动脉高压(PAH)是一种高增殖、抗凋亡的疾病,其有丝分裂增强。动力相关蛋白(Drp1)必须与衔接蛋白形成复合物才可引发分裂。在实验性PAH上,Drp1诱导的分裂已用作治疗靶点。近期研究人员发现了两种新的Drp1衔接蛋白,大小为49和51kDa的线粒体动力蛋白(MiD49和MiD51),Kuang-Hueih Chen等人对其在正常的血管细胞中的作用以及其在PAH的异常情况进行探究。研究人员在肺动
研究人员在肺动脉平滑肌细胞(对照6例、PAH8例)和肺段(对照6例、PAH6例)中检测MiD49和MiD51的表达水平,并在人类和啮齿类PAH肺动脉平滑肌细胞中评估其对细胞增殖、细胞周期和细胞凋亡的影响。同时检测参与MiD表达调控的microRNA(miR-34a-3p)的表达水平,并研究其在PAH的病理过程中如何调控MiDs。
MiD在PAH肺动脉平滑肌细胞中的表达增加,导致Drp1介导的有丝分裂加速,增加细胞增殖、减少细胞凋亡。沉默MiDs(但不干扰其他Drp1结合伴侣,分裂1或线粒体分裂因子)的表达可促进线粒体融合,并通过细胞外信号调节激酶1/2-和细胞周期依赖性激酶4-依赖性方式使细胞分裂周期停滞在G1期。在正常细胞过表达MiDs可引起分裂,再现PAH表型。降低MiR-34a-3p的表达可导致MiD表达上调。在PAH患者和PAH的预临床模型中,循环miR-34a-3p的表达量均降低。沉默MiDs或增强miR-34a-3p的表达量均可抑制实验性PAH。
在正常情况下,MiDs调节Drp-1介导的细胞分裂,但在患病情况下,MiDs上调增强有丝分裂,导致病理性增殖和抗凋亡。miR-34a-3p信号通路为PAH提供了新的治疗靶点。
原始出处:
Kuang-Hueih Chen,et al. Epigenetic Dysregulation of the Dynamin-Related Protein 1 Binding Partners MiD49 and MiD51 Increases Mitotic Mitochondrial Fission and Promotes Pulmonary Arterial Hypertension. Circulation. 2018;https://doi.org/10.1161/CIRCULATIONAHA.117.031258
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#动脉高压#
27
#重要作用#
36
#有丝分裂#
39
#伴侣#
31
肺动脉高压表面是罕见病,事实上临床上并不少见,治疗药物虽然有一些,但是整体仍然不理解,可能未来需要采用综合治疗措施。
61
学习了,长知识
71
学习了,谢谢分享
73
学习了,谢谢分享。
65