英国首例机器人心瓣膜手术:人机偶合不良,导致患者死亡
2018-11-09 全球人工智能 全球人工智能
三年前震惊全球医疗界的机器人手术致死案,有了最新进展。 2015年2月,英国首例机器人心瓣修复手术进行。原本是一场最尖端医疗AI技术的展示,没想到却成了一场鲜血四溅的惨案。 机器人把病人的心脏“放错位置”,还戳穿大动脉;机械臂“乱动”打到医生的手;医生之间的交流全靠“吼”,因为机器人主机发出的声音过于嘈杂…… 最终,接受手术的患者在术后一周去世,英国首例机器人心瓣修复手术以失
三年前震惊全球医疗界的机器人手术致死案,有了最新进展。
2015年2月,英国首例机器人心瓣修复手术进行。原本是一场最尖端医疗AI技术的展示,没想到却成了一场鲜血四溅的惨案。
机器人把病人的心脏“放错位置”,还戳穿大动脉;机械臂“乱动”打到医生的手;医生之间的交流全靠“吼”,因为机器人主机发出的声音过于嘈杂……
最终,接受手术的患者在术后一周去世,英国首例机器人心瓣修复手术以失败告终。
前几天,负责手术的主刀医生、麻醉师等多人进行了听证,这场悲剧结果逐渐水落石出。而从医生口中还原出的当时场景来看,机器人“暴走”的背后,可能还有人为因素。
机器人控制台传输信号弱,血液溅到摄像头
由于是全国首例心脏瓣膜手术,手术室气氛非常紧张。
在手术过程中,机器人控制台传输信号声音非常小,而且质量不佳,主刀医生Sukumaran Nair和助理医生Thasee Pillay之间的交流变得非常困难,术中医生之间的沟通和交流不得不靠彼此扯着嗓门大喊。

出现事故的机器人手术设备(资料图)
更糟糕的是,机器人在手术过程中甚至打到了手术室的一位助理人员的手臂,助理医生Pillay发现,由机器人操作的病人心脏的缝合位置和方式都不对,必须拆除缝线,重新缝合,这样一来就需要更长的时间。
Pillay 还发现,患者的主动脉膈膜受损,而且术中出血溅到了手术机器人的摄像头上,这使得主刀医生Nair已经看不清病人心脏创口缝合的具体情况了。
无奈之下,Nair和助理便由机器手术转为传统“人工”手术。然而,他们发现此时Pettitt心脏的缝合线纵横不齐,需要重新修补时,患者的心脏已然处于非常“衰弱”的状态了。
结果,一周后的2015年3月3日,病人最终由于多器官衰竭逝世,享年69岁。
人祸还是机器背锅?主刀医生承认犯了两个错
这次手术的主刀医生Nair曾在印度和伦敦接受过专业训练,此前曾在剑桥的Papworth医院工作。最近,在出席听证会时他说,自己现在在苏格兰工作,已经不再进行机器人手术。

Sukumaran Nair
Nair本周二出席听证会时,承认自己在使用操作医用机器人上经验不足,操之过急,“还没学会走路,就想学会跑”。
“我向他明确表示,他将成为第一个由机器人进行手术的二尖瓣修复患者。“我曾向他解释过风险。我承认我没有告诉他,作为第一个机器人手术的二尖瓣病人的风险将会更大。”Nair说。
当被问及他是否热衷于机器人二尖瓣置换手术时,Nair说:“在一个国家开发这项技术,是作为一名创新型外科医生希望做的事情。”
但是,Nair也承认在手术之前已然犯下俩个错误。
第一,Nair并没有完全掌握如何操作机器。他承认,在手术之前并没有完成操作的培训课程,就好比“在学会走路之前就想要跑”。
第二次,Nair也没有告知患者Pettitt,他将是英国国内首位接受机器人修复二尖瓣手术的患者,手术存在较高风险,采用传统手术方法存活率会更高。
而手术过程当中,Nair和他的助理Pillay表示,由于机器总是会发出“刺耳”的声音,导致他俩无法用麦克风正常交流,于是他俩不得不提高嗓门大声沟通,更不要提集中注意力了。
雪上加霜的是,当出现问题,他们转头正要向原本应该在场的两位机器指导人员求助时,却发现他俩已经不在场了。Nair本以为他俩是去楼下喝咖啡,而事实上,俩人已经离开医院在回家的路上了。
外科机器人界的波士顿动力,给500万患者做了手术
这次医疗事故中的那台机器人型号为“达芬奇”,是美国加州公司Intuitive Surgical的产品。这台机器人主攻微创手术,被《福布斯》网站称为目前市面上“最成功的手术机器人”。

“达芬奇”最早在2000年获美国食品药品监管局(FDA)的认可,早已实现落地应用。截至2018年10月,已有4000多台“达芬奇”手术系统在全球范围内实现临床使用,有超过500万患者接受过“达芬奇”参与的手术治疗。
英国《每日邮报》称,今年10月一位接受了“达芬奇”机器人手术的患者术后康复得比人工手术还要快。
达芬奇机器人由三部分组成:外科医生控制台、床旁机械臂系统、成像系统。据介绍,在运用“达芬奇”手术系统进行外科手术中,透过机器手臂的协助,外科医师只要坐在控制台,看着手术部位的三度空间影像并进行遥控,机器人手臂的灵巧程度不输人手,还可避免人手会颤抖的情形。
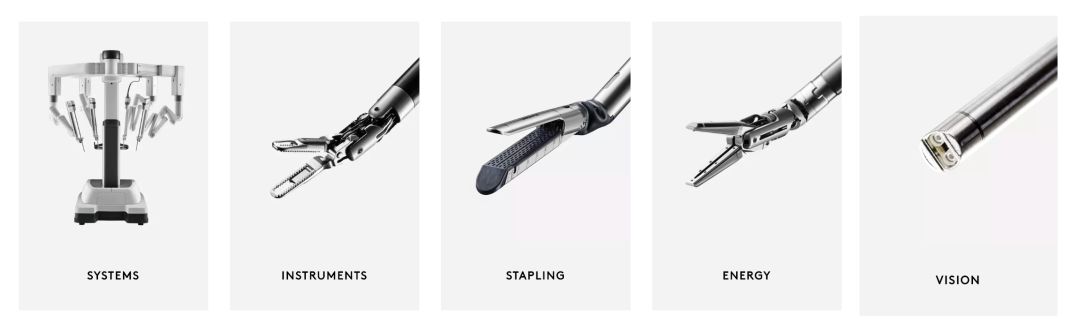
据四川大学华西医院去年的官方介绍,与传统微创手术系统相比,“达芬奇”优势明显:
1.突破了人眼局限,可以进入人体内部,手术视野放大了20倍,为主刀医生呈现患者体腔内三维立体高清影像。手术者目视区域为三维立体影像,这保证了解剖、游离等基本动作的精确性,使分离更彻底、更安全。
2. 突破了人手局限,机器人有7个可旋转540°的手术器械,可以模拟人手腕的灵活穿行,在人手不能触及的狭小空间也能精准操作,具有人手无法比拟的稳定性和精确度,还可以滤除不必要的颤动,超越了人手的精确度;
3.达芬奇机器人手术切口小、创口仅为几个在1厘米左右戳孔,创伤小、出血少、恢复快,大大缩短术后住院时间;
4. 提高安全性,机器人有实时监控系统保证了手术的安全,杜绝误操作的发生。
可以说,达芬奇已经在外科机器人市场中占据着垄断地位,是“外科机器人界的”波士顿动力。
达芬奇机器人已经进入中国,谷歌也涉足
目前,中国也已引进“达芬奇”机器人,有报道称,目前在中国大陆已经有70多台“达芬奇”手术系统在临床使用。
复兴医疗官网介绍,美中互利医疗有限公司(CML)代理的 “达芬奇手术机器人” 是唯一一个已经获得美国 FDA、中国国家食品药品监督管理总局许可上市的微创腔镜外科手术机器人产品,2017年,美中互利达芬奇手术机器人在中国大陆及香港地区手术量超过28000台,较2016年增长约46%。
达芬奇机器人的成功也吸引其他公司想从市场分得一杯羹。
2015年3月,强生官方博客宣布,其旗下一家生产医疗设备的公司 Ethicon 未来将会和 Google X 实验室的生命科学部门宣布成立一家名为VerbSurgical的初创公司,目的是合作研制辅助手术机器人,令医生、病人乃至整个医疗系统都受益。这两家公司的合作加速了医疗设备智能化的过程。
在国内,Intuitive Surgical还在上海成立合资公司直观复星,共同研发和生产用于肺癌早期诊断和治疗的微创手术机器人产品。
今年11月6日,在上海举行的进博会上,来自北京、贵州、河北、云南、新疆等多个省市的21家三级甲等医院与直观医疗达成了达芬奇手术机器人的采购意向,总金额超过了6000万美元。
参考资料
1. https://www.telegraph.co.uk/news/2018/11/05/heart-surgeon-turned-training-pioneering-robot-used-operation/
2. https://www.telegraph.co.uk/news/2018/11/08/tougher-rules-demanded-robotic-surgery-catalogue-errors-leads/
3. https://www.dailymail.co.uk/news/article-6363243/Pioneering-robot-KNOCKED-medics-hand-middle-heart-operation.html
4. http://www.cd120.com/dfqss/80812.jhtml
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#瓣膜手术#
40
#患者死亡#
25
#机器人#
31
#机器#
23
#瓣膜#
29
了解一下,谢谢分享!
52