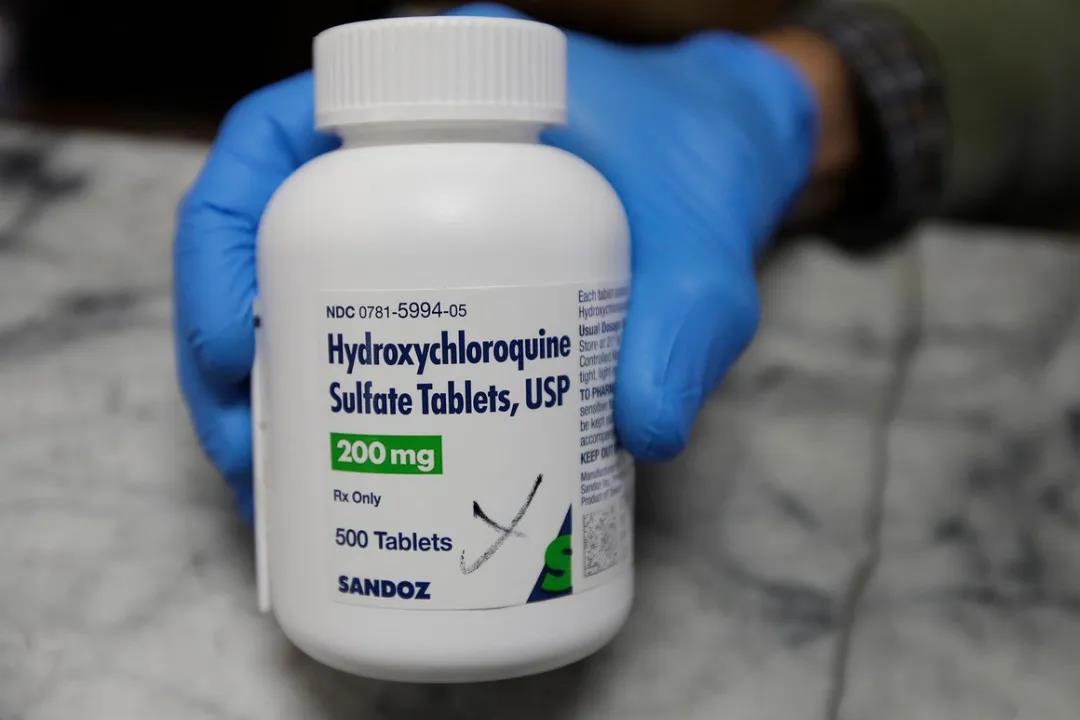
Lancet发布迄今大规模观察性研究,羟氯喹/氯喹治疗COVID-19无益,反而增加死亡风险
2020-05-27 医咖会 医咖会
近期关于羟氯喹/氯喹的研究发布了不少,5月22日,Lancet也发表了一项研究,是迄今针对羟氯喹/氯喹规模最大的一项观察性研究。
近期关于羟氯喹/氯喹的研究发布了不少,5月22日,Lancet也发表了一项研究,是迄今针对羟氯喹/氯喹规模最大的一项观察性研究,与既往研究结果较为一致,显示羟氯喹/氯喹单药或与大环内酯联用对COVID-19住院患者无益处,反而增加了院内死亡率和室性心律失常的风险。
原文链接:
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)31180-6/fulltext#seccestitle170
研究方法
这是一项跨国注册研究,收集了六大洲(北美、南美、欧洲、非洲、亚洲、澳洲)671家医院的数据。研究纳入了在2019年12月20日至2020年4月14日期间的Covid-19住院患者。
治疗组为确诊48小时内接受了以下任一种治疗的患者:氯喹、氯喹+大环内酯、羟氯喹、羟氯喹+大环内酯;对照组没有接受以上治疗。研究的主要结局是院内死亡率,新发室性心律失常(非持续性或持续性室性心动过速或室颤)。
基线特征
研究纳入了96032名Covid-19住院患者(图1)。所有纳入患者均于2020年4月21日前出院或死亡。研究期间没有完成治疗疗程的患者未被纳入分析。最终的研究队列包括来自北美的63315名患者(65.9%),欧洲的16574名患者(17.3%),亚洲的7555名患者(7.9%),非洲的4402名患者(4.6%),南美的3577名患者(3.7%),澳大利亚的609名患者(0.6%)。治疗组有14888例患者,对照组有81144例患者。

图1 纳入流程
患者的平均年龄是53.8岁(SD 17.6),44426名(46.3%)为女性,平均BMI是27.6 kg /m2(29 510[30.7%]名肥胖患者,BMI≥30 kg/m2)。
30198例(31.4%)合并有高脂血症,25810例(26.9%)有高血压,13260例(13.8%)有糖尿病,3177例(3.3%)有COPD。16553例(17.2%)曾经吸烟,9488例(9.9%)目前吸烟。关于心血管疾病史,12137例(12.6%)有冠心病史,2368例(2.5%)有充血性心力衰竭病史,3381例(3.5%)有心律失常病史。
平均住院时长为9.1天(SD 6.4),院内总死亡率为11.1%(10698/96032)。38927例(40.5%)患者使用了抗病毒药物,最常见的是利托那韦+洛匹那韦(12304,31.6%)、利巴韦林(7904,20.3%)、奥司他韦(5101,13.1%)。6782例(17.4%)患者使用了2种以上抗病毒药物联合治疗。
治疗情况
从入院到确诊的中位时间为2天(IQR 1-4)。治疗组中,1868例接受了氯喹单药治疗,3016例接受了羟氯喹单药治疗,3783例接受氯喹+大环内酯治疗,6221例接受羟氯喹+大环内酯治疗。
治疗药物的平均每日剂量和持续时间为:氯喹组:765 mg(SD 308),6.6天(2.4);羟氯喹组:596 mg(126), 4.2天(1.9);氯喹+大环内酯组:790 mg(320),6.8天(2.5);羟氯喹+大环内酯组:597 mg(128),4.3天(2.0)。
主要结果
未发现组间在基线特征或合并症上有明显的差异。与对照组相比,治疗组的室性心律失常更为常见。治疗组死亡率高于对照组。
院内死亡率的独立预测因子如图2所示。年龄、BMI、黑人或西班牙裔(白人作为对照)、冠心病、充血性心力衰竭、心律失常史、糖尿病、高血压、高脂血症、COPD、目前吸烟、免疫抑制状态与死亡风险升高存在相关性。女性、亚裔、使用ACEI(非ARB)、他汀类药物与死亡风险降低存在相关性。
与对照组的死亡率(9.3%)相比,羟氯喹组(18.0%;HR 1.335;95% CI 1.223-1.457),羟氯喹+大环内酯组(23.8%;1.447;1.368-1.531),氯喹组(16.4%;1.365;1.218-1.531),氯喹+大环内酯组(22.2%;1.368;1.273-1.469)与院内死亡风险增加独立相关。
室性心律失常的独立预测因子见图3。冠心病、充血性心力衰竭、心律失常史、COPD与室性心律失常风险增加独立相关。与对照组(0.3%)相比,羟氯喹组(6.1%;HR 2.369;95% CI 1.935-2.900),羟氯喹+大环内酯组(8.1%;5.106;4.106-5.983),氯喹组(4.3%;3.561;2.760-4.596),氯喹+大环内酯组(6.5%;4.011;3.344-4.812)与院内新发室性心律失常的风险增加独立相关。
总结
这项针对COVID-19住院患者进行的跨国真实世界研究发现,羟氯喹/氯喹联合或不联合大环内酯无获益证据,反而会增加室性心律失常和院内死亡的风险。这些发现表明,这些用药方案不应在临床试验之外使用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#大规模#
34
#Lancet#
31
#死亡风险#
33
#观察性研究#
30
顶刊就是不一样,质量很高,内容精彩!学到很多
47